Anterior chamber bevacizumab for rubeotic glaucoma secondary to retinal artery occlusion☆
Financial support (grants) and proprietary interests: None.
- DOI
- 10.1016/j.artres.2009.06.001How to use a DOI?
- Keywords
- Anterior chamber; Bevacizumab; Rubeotic glaucoma; Central retinal artery occlusion
- Abstract
A 73-year-old Caucasian female, presented with sudden loss of vision in the right eye due to a central retinal artery occlusion (CRAO). The patient presented acutely 10-weeks later with a painful right eye due to rubeosis; intraocular pressure (IOP) was 67mmHg. A single anterior chamber injection of bevacizumab was performed as an adjunct combination therapy for her neovascularisation. Informed consent to the patient included a detailed explanation of the medication licensing status. 1-week post injection the cornea was clear and there was less rubeosis. Pan-retinal photocoagulation (PRP) was performed and 1 month later there was a marked reduction in rubeosis iridis. At 6 months follow up the patient remains comfortable on prednisolone acetate 1% OD and atropine 1% OD; IOP is 24. As the main trigger for such neovascularisation is retinal ischaemia, the incidence of rubeosis in CRAO is relatively low. Successful combination treatment of rubeosis following CRAO with a single intravitreal injection of anti-VEGF followed by PRP has been reported. In our opinion anterior chamber injection of anti-VEGF may be less invasive than intravitreal delivery. Although there are emerging reports regarding the successful use and efficacy of the anterior chamber route of administration for the treatment of rubeosis from venous occlusion, no such reports have been published following CRAO.
- Copyright
- © 2009 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
We report a unique case of neovascular glaucoma due to central retinal artery occlusion treated with a single anterior chamber injection of bevacizumab as an adjunct combination therapy.
A 73-year-old Caucasian female, presented with sudden loss of vision of 2h duration in the right eye due to a central retinal artery occlusion. Best-corrected visual acuity (VA) was perception of light (PL) in the affected eye and 6/6 in the left. An anterior chamber (AC) paracentesis was performed and intraocular pressure dropped from 18mmHg to 6mmHg. 24h later VA improved to hand movements. The patient had type II diabetes, and had had two cerebrovascular accidents in the past.
Erythrocyte sedimentation rate was normal and ultrasound examination revealed 50% stenosis of the right internal carotid artery. Ten weeks later the patient presented again with severe pain in her right eye due to rubeotic glaucoma. VA was PL and IOP 67mmHg with gross rubeosis iridis and corneal oedema (Fig. 1). Pan-retinal photocoagulation (PRP) was performed on the same day with difficulty due to the corneal oedema and patient discomfort. Six days later the patient was still in pain with raised pressure despite oral acetazolomide and topical anti-hypotensive agents; the IOP was 54mmHg.
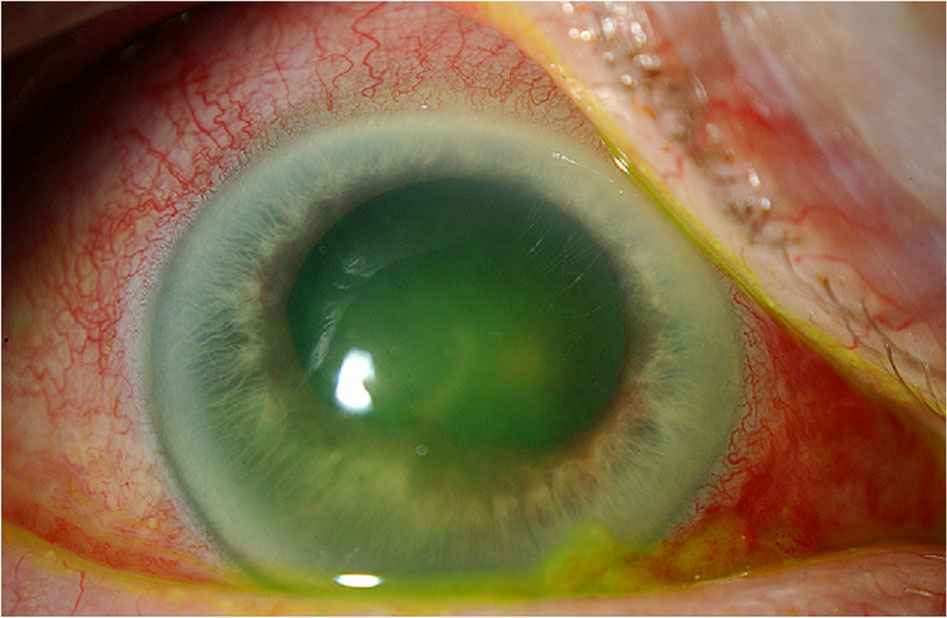
Right eye on presentation.
Following intravenous acetazolomide the IOP reduced to 27 but the corneal oedema persisted. Trans-scleral diode laser cyclo-ablation was then applied under local anaesthetic, which consisted of 20 applications to 270° of ciliary body. (IRIS Oculight Diode Laser System, IRIS Medical Instruments: Mountain View, CA) Two days later IOP was 27 and 1.25mg of bevacizumab injection was given by anterior chamber injection in 0.05ml using sterile technique. The bevacizumab was supplied in a sterile syringe from Moorfields Eye Hospital pharmacy.
Informed consent to the patient included a detailed explanation of the medication’s off-licence status. 1-week later the cornea was clear, there was less rubeosis and the IOP was 7mmHg. Further PRP (2794 burns) was then performed and 1 month later there was a marked reduction in rubeosis iridis (Fig. 2). At 6 months follow up the patient remains comfortable on prednisolone acetate 1% OD and atropine 1% OD; the cornea remains clear and IOP 24mmHg.

Right eye 1 month following treatment.
Central retinal artery occlusion may be due to embolus or thrombosis.1 The prevalence of CRAO is 0.7 in 100,000 population, with subsequent rubeosis occurring in only 15% of such patients.2 As the main trigger for such neovascularisation is retinal ischaemia,3 the incidence of rubeosis in CRAO is relatively low. The treatment of rubeotic glaucoma consists of PRP, which may be used in combination with cyclodiode laser. Vascular endothelial growth factor (VEGF) is produced from hypoxic tissue resulting in neovascularisation responsible for the development of conditions such as proliferative diabetic retinopathy and rubeotic glaucoma. Anti-VEGF monoclonal antibody agents have the potential for novel additional treatment for rubeotic glaucoma by directly affecting the angiogenic process.4
Vatavuk et al 5 reported the successful combination treatment of rubeosis following CRAO with a single intravitreal injection followed by PRP. In our opinion anterior chamber injection of anti-VEGF may be less invasive than intravitreal delivery.6 Although there are emerging and encouraging case reports regarding the use of anterior chamber anti-VEGF in the treatment of rubeosis from venous occlusion,4,7 we are not aware of any such reports following CRAO. Therefore we believe this is a clinical area requiring more study.
Conflict of interest
The authors declare no financial or conflict of interest.
References
Cite this article
TY - JOUR AU - Rajan Bhojwani AU - Simon P. Kelly PY - 2009 DA - 2009/07/05 TI - Anterior chamber bevacizumab for rubeotic glaucoma secondary to retinal artery occlusion☆ JO - Artery Research SP - 122 EP - 123 VL - 3 IS - 3 SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2009.06.001 DO - 10.1016/j.artres.2009.06.001 ID - Bhojwani2009 ER -
