Resurgence of Measles in Europe: A Systematic Review on Parental Attitudes and Beliefs of Measles Vaccine
- DOI
- 10.2991/jegh.k.191117.001How to use a DOI?
- Keywords
- Vaccine confidence; Wakefield; vaccine refusal; measles; vaccine hesitancy
- Abstract
Background and Objectives: Europe has experienced a major resurgence of measles in recent years, despite the availability and free access to a safe, effective, and affordable vaccination measles, mumps and rubella vaccine (MMR). The main driver for this is suboptimal vaccine coverage. The three objectives of this study are to synthesize and critically assess parental attitudes and beliefs toward MMR uptake, to develop strategies and policy recommendations to effectively improve MMR vaccine uptake accordingly, and ultimately to identify areas for further research.
Methods: A systematic review was conducted using primary studies from PubMed, Medline, Embase, and Scopus published between 2011 and April 2019. Inclusion criteria comprised primary studies in English conducted in Europe and studying parental attitudes and behavior regarding MMR uptake. Data were extracted using an inductive grounded theory approach.
Results: In all, 20 high-quality studies were identified. Vaccine hesitancy or refusal were mainly due to concerns about vaccine safety, effectiveness, perception of measles risk and burden, mistrust in experts, and accessibility. Factors for MMR uptake included a sense of responsibility toward child and community health, peer judgement, trust in experts and vaccine, and measles severity. Anthroposophical and Gypsy, Roma, and Traveler populations presented unique barriers such as accessibility.
Conclusion: A multi-interventional, evidence-based approach is vital to improve confidence, competence, and convenience of measles vaccination uptake. Healthcare professionals need an understanding of individual contextual attitudes and barriers to MMR uptake to tailor effective communication. Effective surveillance is needed to identify under-vaccinated populations for vaccination outreach programs to improve accessibility and uptake.
- Copyright
- © 2019 Atlantis Press International B.V.
- Open Access
- This is an open access article distributed under the CC BY-NC 4.0 license (http://creativecommons.org/licenses/by-nc/4.0/).
1. INTRODUCTION
Measles is a highly contagious viral infection that can cause serious illness, life-long complications, and death [1]. In the absence of an immunization program, approximately 95% of individuals would be infected with measles by 15 years of age [2]. Measles is preventable with a safe and effective vaccine [2]. The World Health Organization (WHO) recommends all national immunization programs to include two doses of Measles-Containing Vaccine (MCV). In countries with ongoing measles transmission, the first dose (MCV1) should be administered at 9 months of age, followed by the second dose (MCV2) at 15–18 months [2]. Owing to its high incidence and burden, measles elimination is one of the top priorities of the 53 Member States of the WHO European Region [3]. In 2014, WHO-Europe initiated the European Vaccine Action Plan (EVAP) 2015–2020 [4]. By 2014, the UK had interrupted endemic transmission of measles and was declared eliminated in the UK in 2017 by the European Regional Verification (RVC) for Measles and Rubella Elimination. In England, vaccine coverage of the first Measles, Mumps and Rubella Vaccine (MMR) dose in 5-year-olds reached 95% for the first time in 2016–17. However, high vaccine coverage rates consistently above 95% have not been achieved in Europe even though MMR is freely available. Despite some intermediate successes, Europe is currently experiencing a major measles resurgence [5,6], further propagated by travel and migration [6,7] with low vaccine coverage rates in certain subpopulations [8]. In 2018, 47 of 53 Member States of the WHO European Region reported over 84,000 confirmed measles cases. In Europe, cases rose by 300% during the first 3 months of 2019 compared with the same period in 2018 [9].
Plans-Rubio assessed measles vaccination coverage in the European Union and the WHO European Region from 1980 to 2015 [10]. Despite the general increase in MCV1 coverage throughout Europe from 84% in 1995 to 95% in 2017 [11], a number of European countries continue to have suboptimal coverage below 95%. This is even more problematic regarding the second vaccine dose; in 2017, the WHO European Region had just 90% coverage of MCV2 [12]. The additional vaccination coverage required to establish herd immunity are estimated to range from 0.2% to 18%, demonstrating variation between countries [10]. Plans-Rubio argued that low vaccine coverage is the driving factor for measles persistence in Europe. WHO’s European Observatory on Health Systems report examined barriers to optimal vaccination coverage and found the most significant barrier to be vaccine hesitancy, evident across all European countries [13]. The WHO Strategic Advisory Group of Experts defines vaccine hesitancy as the ‘delay in acceptance or refusal of vaccination, despite availability of vaccination services’ [14]. The WHO highlighted three categories that determine vaccine hesitancy; confidence, complacency, and convenience [14]. Confidence in vaccination is hindered by mistrust in experts and misconceptions. Complacency is influenced by perceived importance of vaccination and is affected by competing life factors. Convenience is driven by circumstantial barriers of vaccination; the availability, affordability, and accessibility of vaccines. These factors can be independent or overlapping, but ultimately impact vaccination uptake.
Fears of serious adverse events by measles vaccination were triggered following Wakefield’s (1998) publication [15] in The Lancet, suggesting a causative link between MMR and autism [16]. His study, funded by lawyers engaged in lawsuits against vaccine-producing companies and using a small and selective population of 12 children in Britain, has since been disproved, discredited, and retracted [17]. Nonetheless, his findings became a global media sensation, fueling publicity amongst anti-vaccination groups and negative press. Fear of autism left persistent negative attitudes toward MMR and resulted in the decline in measles vaccination coverage in the UK from 92% in 1996 to 84% in 2002 [16,18]. Vaccine decision-making is context-specific and heavily reliant upon knowledge and information, attitudes and values, and experiences and emotions [19]. Beliefs concerning vaccination are not simply binary, but rather exist on a continuum of hesitancy, between two extremes from complete acceptance to complete refusal [14]. Vaccine hesitancy may involve selective refusal, delay, or acceptance of vaccination with doubts. Parents play a large role for deciding MMR uptake at the individual and family level. Therefore, this systematic review aims to synthesize parental attitudes and beliefs toward measles vaccine uptake in Europe. Using these findings, we aim to develop strategies and policy recommendations to effectively improve measles vaccine uptake, and identify areas for further research.
2. MATERIALS AND METHODS
We followed the Cochrane guidance to guide the systematic review; the PRISMA checklist can be found in Appendix 1. Initially, preliminary scoping searches were performed over multiple academic databases to find four suitable, comprehensive databases: Medline, Scopus, Web of Science, and Embase. Subsequently, systematic reviews on attitudes toward general vaccine uptake were used to inform MeSH headings and key terms. Additional keywords were added to narrow the search to focus on Europe and measles, as seen in Figure 1. The categorization of countries that constitute Europe differs between United Nations definitions, WHO regions, and EU/EEA areas. To remain consistent to Plans-Rubio’s study, the 53 Member States of the WHO European Region were used to define the geographical scope. Therefore, MeSH headings were supplemented to ensure all countries of the WHO European Region were included.

Search string used for Medline database.
Filters were used to display only primary studies, as the aim is to explore parental perspectives; these were mainly qualitative studies, however also included quantitative surveys and questionnaires. Next, the search was restricted to articles in English published after 2011 due to the large number of results. Owing to differences between databases, each search string was adapted, yet kept as consistent as possible to ensure congruity between searches. The literature search was conducted between 1 March and 23 April 2019.
In all, 869 papers were identified, 562 remained after duplicates were removed. A two-stage systematic screening was then done using the exclusion and inclusion criteria in Table 1, which were developed iteratively throughout the searching process. First, two reviewers independently screened the titles and abstracts using the inclusion and exclusion criteria. The remaining 84 studies underwent full-text screening using the same criteria. In case the two researchers disagreed, a third researcher would have been consulted, however, no disagreement occurred. A consistency check was done by repeating the individual screening process and no inconsistencies were found. Finally, the Critical Appraisal Skills Programme [20] was used to assign a quality score out of 10. The majority of studies (n = 18) scored between 7 and 9, and the lowest included studies (n = 2) scored 6 out of 10. The lowest quality outlier (4/10) was excluded as it was a pilot study. The quality score of each paper is shown in Table 2. The full screening process is depicted in Figure 2. Ethical approval was obtained from the University of Edinburgh School of Social and Political Science Ethics Review Committee (Ref: 29/01/19).
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Study design | Title or abstract must mention measles or measles vaccination. | Studies published before 2011. |
| Title or abstract must mention ‘vaccine uptake’, ‘attitudes’, ‘acceptance’, ‘hesitancy’, or ‘refusal’. | Studies not in English. | |
| Primary data. | Secondary data. | |
| Focus groups, in-depth interviews, questionnaires, and surveys. | Purely quantitative data. | |
| Study population | Parental population group. | Study population of only children, adolescents, healthcare workers, or students. |
| Studies conducted only in Europe. | Studies conducted outside Europe. | |
| Research topic | Studies focusing on attitudes or beliefs about measles vaccine. | Studies focusing primarily on effectiveness of interventions, epidemiological mapping, or serological research. |
Exclusion and inclusion criteria
| References | Publication year | Study country | Research aim | Data collection | Population group | Data analysis | CASP | |
|---|---|---|---|---|---|---|---|---|
| 1 | Brown, Fraser, Ramsay et al. [40] | 2011 | UK | To explore attitudes and predictors of MMR catch-up vaccine uptake. | Self-administered questionnaire | 365 UK parents whose children aged 5–18 years had received <2 MMR doses before 2008. | Quantitative analysis | 7/10 |
| 2 | Brown, Long, Ramsay et al. [23] | 2012 | UK | To explore parents’ MMR decision making since 2004. | Semi-structured interviews | 24 mothers planning to accept, postpone or decline the first MMR dose for their 11–36 month old children. | Grounded theory approach | 8/10 |
| 3 | Byström, Lindstrand, Likhite et al. [28] | 2014 | Sweden | To explore facilitators and barriers to MMR vaccination among parents living in anthroposophical communities in Sweden. | In-depth interviews | 20 parents in an anthroposophical community. | Qualitative content analysis | 7/10 |
| 4 | Camerini, Diviani, Fadda et al. [36] | 2019 | Switzerland | To identify predictors of parents’ intention to adhere to official MMR vaccination recommendations. | Self-administered questionnaire | 554 parents of middle school students aged 13 to 15. | Quantitative analysis | 8/10 |
| 5 | Fadda, Depping and Schulz [34] | 2015 | Switzerland | To understand what drives parents’ decision to vaccinate against measles, with a focus on vaccination literacy and psychological empowerment. | Semi-structured interviews | 20 parents, of at least one child under 1 year, of permanent residence in Ticino. | Inductive thematic analysis | 8/10 |
| 6 | Fadda, Galimberti, Carraro et al. [38] | 2016 | Italy | To gain insights from parents residing in a low MMR uptake area on what constitutes feelings of empowerment in the decision they have to make on their child’s MMR vaccination. | Focus group interviews | 24 mothers and 4 fathers of children for whom the MMR vaccination decision was still pending. Parents residing in Italy, of at least one child ages <1 year. | Inductive thematic analysis | 7/10 |
| 7 | Giambi, Fabiani, D’Ancona et al. [29] | 2018 | Italy | To estimate vaccine hesitancy and investigate its determinants among parents of children aged 16–36 months. | Questionnaire | Parents of children aged 16–36 months. 3130 questionnaires used in analysis. | Multivariable logistic regression | 9/10 |
| 8 | Gross, Hartmann, Zemp et al. [35] | 2015 | Switzerland | To investigate how Swiss parents use natural development of the child to explain their critical attitudes towards immunisation against measles and other childhood diseases. | Semi-structured interviews | 32 interviews with parents of children between 0 and 16 years who decided not to fully immunise their children. | Qualitative content analysis | 9/10 |
| 9 | Jama, Ali, Lindstrand et al. [25] | 2018 | Sweden | To explore factors influencing the decision of Somali parents living in 2 districts of Stockholm, Sweden, on whether to vaccinate their children with MMR. | In-depth interviews | 13 mothers of at least one child aged 18 months to 5 years. | Qualitative content analysis | 8/10 |
| 10 | Johnson and Capdevila [26] | 2014 | UK | To explore the ways mothers make sense of and work with varying advice and information within their contexts and circumstances, in relation to MMR and vaccinations. | Focus group interviews | 5 mothers of preschool children between ages 12 and 18 months. | Thematic analysis | 6/10 |
| 11 | Kennedy, Brunton and Hogg [32] | 2013 | UK | To explore vaccination views in Scotland amongst parents, teenage girls and health professionals across 3 controversial vaccines and consider contextual influences on decision-making. | Semi-structured interviews and focus group discussions. | 51 health professionals, 15 parents and 8 teenage girls aged 12–15 years. | Iterative thematic analysis | 8/10 |
| 12 | Klomp, van Lier and Ruijs [27] | 2014 | The Netherlands | To get an insight into the attitudes towards childhood vaccination of parents with children attending anthroposophical schools. | Questionnaire | 458 parents of children aged 4–18 years at anthroposophical schools in Gelderland. | Quantitative analysis | 6/10 |
| 13 | Kriwy [39] | 2012 | Germany | To investigate parental decisions to vaccinate their children against MMR. | Database analysis and surveys | Database: 9270 children Survey: 464 parents and 136 physicians. | Quantitative analysis | 7/10 |
| 14 | McHale, Keenan and Ghebrehewet [33] | 2015 | UK | To identify factors that continue to affect MMR uptake rates and consider key issues related to parents or carers of confirmed measles cases. | Semi-structured interviews | Parents or carers of 47 unvaccinated measles cases aged between 13 months and 9 years. | Thematic analysis | 9/10 |
| 15 | Newton and Smith [22] | 2017 | UK | To explore Gypsy, Roma and Traveller parents’ beliefs about childhood immunisation, the risks of immunisation and nonimmunisation, obstacles to and facilitators of immunisation and views on increasing immunisation levels. | Focus group interviews | 16 Gypsy and Traveller women with pre-school aged children. | Thematic analysis | 8/10 |
| 16 | Restivo, Napoli, Marsala et al. [31] | 2014 | Italy | To evaluate the refusal level of first MMR dose, and investigate sociodemographic characteristics associated with refused vaccination and reasons reported by parents for their child’s immunisation status. | Questionnaire | 443 parents who accepted/refused first dose of MMR vaccination for children in 13–20th month. | Quantitative analysis | 7/10 |
| 17 | Rey, Fressard, Cortaredona et al. [41] | 2018 | France | To estimate the prevalence and socio-demographic correlates of vaccine hesitancy in sub-groups of the French population. To investigate the association of vaccine hesitancy with both vaccine uptake and perceived risk-benefit balance for four vaccines. | Telephone survey | 3938 parents between 15–75 years: Parents of children 1–15 Parents of adolescent girls 11–15 Individuals aged 65–75. |
Quantitative analysis | 8/10 |
| 18 | Smith and Newton [24] | 2016 | UK | To explore the issues Gypsy, Roma and Traveller (GRT) parents consider when making vaccination decisions in the context of wider social, ideological, material and practical considerations. | Focus group interviews | 5 focus groups of 16 GRT women, who had 35 children between them. 13 were not immunised. | Thematic analysis | 8/10 |
| 19 | Walsh, Thomas, Mason et al. [30] | 2014 | UK | To investigate parents’ decision on whether to accept MMR. | Self-administered questionnaire | 66 parents/guardians of children aged 2 who have not received MMR. | Quantitative analysis | 8/10 |
| 20 | Weiss, Schröpfer and Merten [37] | 2016 | Switzerland | To investigate how patterns of parental attitudes are linked to the decision-making process for or against MMR vaccination. | Questionnaire | 189 parents of children <36 months. | Quantitative analysis | 9/10 |
A summary of study characteristics
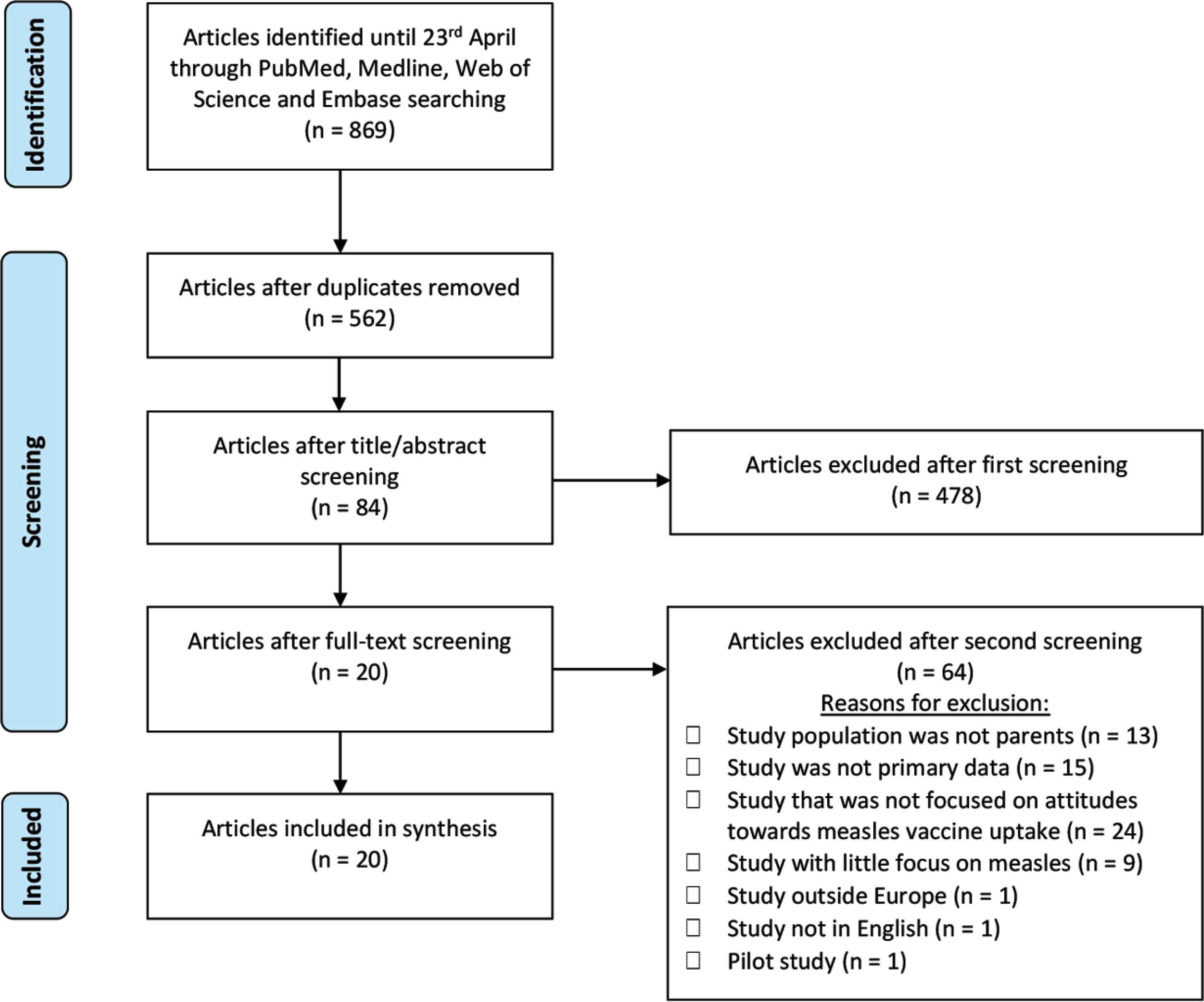
PRISMA flow diagram of the complete search process.
2.1. Synthesis
The remaining 20 studies were analyzed (Table 2). An inductive grounded theory approach was used for data extraction, whereby the researchers progressively identified themes from the data to create an explanatory framework [21]. This approach is appropriate because it allows systematic extraction of novel findings without compromising the richness of the data with preconceived themes. Data were taken only from the findings/results section to remain consistent with primary-order outcomes and to avoid reproduction of authors’ interpretations. Distinguishing between complete acceptors and rejectors, and vaccine-hesitant parents was not always clear-cut. Therefore, the terms ‘acceptors’ and ‘rejectors’ will be used in reference to parents’ complete acceptance or refusal of MMR, whereas ‘vaccine-hesitant’ parents represent attitudes between the two. Both reviewers individually noted the main key themes presented throughout the 20 remaining studies. There were no discrepancies in determining key themes and sub-themes as these were inductively categorized throughout screening.
3. RESULTS
The six key themes identified were measles vaccine factors, measles factors, trust factors, social factors, practical factors, and knowledge factors.
3.1. Characteristics of Studies
The final review included 20 studies, which were conducted in seven countries across the WHO European Region; UK (n = 8), Switzerland (n = 4), Italy (n = 3), Sweden (n = 2), Netherlands (n = 1), Germany (n = 1), and France (n = 1) (Table 2). These represent countries with a range of measles incidence, from Italy with a measles incidence of 83.7 per 1 million population, the fourth highest in Europe in 2017, to the Netherlands with 0.9 per 1 million population. Eleven studies used qualitative methods, such as semi-structured interviews or focus-group discussions. The remaining nine studies used questionnaires or surveys, followed by quantitative analysis.
Participants were mainly mothers [22–26], and also included parents with anthroposophical world views [27,28]; some studies included Gypsies, Roma, and Traveler (GRT) parents [22,24], with a history of nomadism and temporary residency, and long-term resident Somali mothers living in Europe [25]. Most studies used a retrospective design in which attitudes and predictors were assessed after they had made their vaccination decision using subjective self-reported behavior. Table 2 summarizes the study characteristics. Tables 3 and 4 summarize the themes that encouraged MMR uptake and non-uptake, respectively.
| Themes | Sub-themes | Studies |
|---|---|---|
| Vaccine factors | Provide herd immunity | 1–5, 7, 10 |
| Protect the child | 3, 4, 7, 19, 20 | |
| Belief in vaccine efficacy | 4, 15, 18, 19 | |
| Belief in vaccine safety | 1, 6, 19 | |
| Benefits outweigh risks | 19 | |
| Can easily treat complications of vaccine | 20 | |
| Child mixing with unimmunized people | 2 | |
| Measles factors | Concern about severity of measles | 1, 2, 18, 19, 20 |
| Concern about susceptibility to measles | 4, 15 | |
| Lack of time/ability/competence to deal with measles | 3 | |
| Trust factors | Trust in healthcare workers, experts, or government | 2, 3, 5, 6, 7, 9, 19, 20 |
| Trust in God | 9 | |
| Social factors | Social desirability | 1, 2, 4, 10 |
| Responsibility over child | 10, 11, 19 | |
| Decision to vaccinate is intuitive | 3, 5, 10 | |
| Follow social norm | 5 | |
| Guilt for non-vaccination | 2 | |
| Practical factors | Follow recommendations | 2–4, 7, 10 |
| Little time to make informed decision | 10 | |
| Knowledge factors | Influence from peers/family | 1, 9 |
| Satisfied with information | 1 |
Themes that emerged promoting MMR vaccine uptake
| Themes | Sub-themes | Studies |
|---|---|---|
| Vaccine factors | Fear of vaccine side effects | 2–9, 13, 15, 17, 19, 20 |
| Doubts of vaccine safety | 2, 3, 6, 7, 9–12, 14 | |
| High risk compared to benefit from vaccine | 7–9, 12, 13, 15, 17, 18 | |
| Experience (self/peers) of vaccine side effects | 2, 4, 5, 9, 11, 14, 18 | |
| Vaccination given too young | 2, 3, 7–9, 15, 18 | |
| Fear of combined vaccines | 7, 11, 15, 18, 19 | |
| Immune overloading | 2, 7, 8, 12 | |
| Doubts of vaccine efficacy | 2, 8, 12, 17 | |
| Fear of vaccine constituents | 2, 7, 10, 14 | |
| Intrusion/invasive procedure | 8, 15, 18, 20 | |
| Doubts of necessity of vaccine | 7, 12 | |
| Family history of autism | 19 | |
| Measles factors | Lack of severity of measles | 4, 5, 7–9, 13–15, 18, 20 |
| Perceived low susceptibility to measles | 4, 5, 8, 9, 15 | |
| Measles helps child development | 3, 8, 19 | |
| Competence to cope with measles | 3 | |
| Trust factors | Mistrust in healthcare workers/experts/government | 2, 3, 5, 6, 10, 11, 18, 19 |
| Bad experience/relationship/communication with healthcare workers | 9, 10, 13, 14, 18 | |
| Fear of commercial motivation | 2, 7, 20 | |
| Social factors | Natural immunity preferred | 2, 3, 5, 8, 12, 19, 20 |
| Alternative medicine preferred | 3, 12–14 | |
| Right to autonomous decision | 3, 5, 16, 18 | |
| Healthy lifestyle measures are sufficient to treat/prevent | 2, 5, 7, 8 | |
| Decision requires more time | 3, 6 | |
| Disease is a natural part of life | 3 | |
| Fear of judgement from peers | 9 | |
| Practical factors | Contradictions to vaccination | 7, 14–16, 18 |
| Access to clinics | 15, 16, 18 | |
| Temporary residence | 14, 15, 18 | |
| Forgetfulness | 7, 14, 15 | |
| Competing priorities | 15, 18 | |
| Cost of individual vaccine | 15, 18 | |
| Did not receive timely vaccination invitation | 1, 7 | |
| Vaccine not offered | 14 | |
| Knowledge factors | Insufficient information | 2, 7, 9, 10, 13, 14, 16, 18 |
| Misinformation online/media | 11, 14, 16, 18, 19 | |
| Lack competence to make decision | 5, 6 | |
| Discordant information | 7, 10 | |
| Lay knowledge from family/peers | 15, 20 | |
| Advised against/cautioned by healthcare provider | 7, 11 |
Themes that emerged promoting MMR vaccine hesitancy or refusal
3.2. Vaccine Factors
3.2.1. Side effects
The most common reason for hesitancy or refusal was concern about adverse effects, revealed in 13 of 20 studies. This was mentioned by participants in relation to fear of autism in 10 studies [22–26,29–33] across three countries (UK, Italy, and Sweden). Rejectors and vaccine-hesitant parents were more likely to perceive adverse effects as highly probable and severe [29,34]. Similarly, vaccine-hesitant parents in Switzerland believed the risks of vaccination were worse than measles itself [35].
In contrast, acceptors believed adverse effects were unlikely and non-severe [34]. GRT mothers who chose to vaccinate believed the risks of vaccination were less than the risks surrounding measles infection, and doubted the link between MMR and autism [22]. A UK study found that parents with a family history of autism were more likely to be rejectors, but those with a healthy vaccinated child were more likely to continue vaccination [30].
3.2.2. Effectiveness
A Swiss study revealed that perceived vaccine effectiveness was the only significant predictor for vaccination [36]. Further studies showed rejectors to be the only population to question vaccine effectiveness and believe that MMR protection was incomplete [23,27,35]. However, acceptors in a Swedish study argued that the only reason for failure of vaccine effectiveness would be if not enough people vaccinate [28].
3.2.3. Vaccination
Some rejectors and vaccine-hesitant parents were concerned about combined and co-administered vaccines, and therefore preferred spacing vaccination [22,24,29]. Some believed that combination vaccines can overload the immune system [24,37]. However, in GRT populations, the cost of separate vaccination was a barrier to uptake [22]. Two Swiss studies revealed the belief that vaccines are an artificial, unnecessary intrusion into the development of the natural immune system [35,37]. Similarly, GRT rejectors believed vaccination was traumatic, causing unnecessary distress to the child [22].
3.2.4. Age
A common finding in local, anthroposophical, and GRT populations showed vaccine delay due to the belief that vaccination was given too young [22,24,27–29]. Some GRT mothers believed that immune systems would mature with age, and reduce risks of vaccination [24]. However, some mothers from studies in the UK and Sweden used stages of development to inform timeliness of uptake, and therefore delayed vaccination until the child began speaking and socializing normally [23,25].
3.3. Measles Factors
3.3.1. Severity
Acceptors in a Swedish anthroposophical community frequently believed that measles is severe [28]. These parents perceived measles as a burden, so vaccinated due to lack of time, ability, or self-efficacy to care for their sick children [28]. A few, highly educated acceptors in a Swiss study also cited the possible serious consequences of measles [34]. However, parents’ views on measles severity were often rooted in experience rather than population-level statistics [23,24,28,34,35]. For example, one GRT mother’s experience of her son suffering from measles was enough impetus to vaccinate [24]. On the other hand, across the UK, Sweden, and Switzerland, rejectors perceived measles to be mild, treatable, or preventable through other routes, making vaccination unnecessary [23,28,34,37].
3.3.2. Likelihood of infection
Some hesitant parents in a Swiss study believed the probability of measles infection was low [34]. Vaccine-hesitant parents in an Italian study perceived low risk of measles infection because of non-mandatory vaccination [31]. However, some were motivated to vaccinate depending on situational likelihood of infection, such as if their child was mixing with unimmunized people, or during outbreaks [23,28]. Some GRT acceptors believed their child was more prone to contracting diseases due to frequent bouts of illness in these communities [22,24].
3.3.3. Natural immunity
The benefits of developing natural immunity were felt more strongly by rejectors in a British study, although it was mentioned by both acceptors and rejectors [23]. Many rejectors, including anthroposophical parents, believed that being infected with measles is a natural, meaningful stage of a child’s development [28,35].
3.4. Trust Factors
3.4.1. Healthcare professionals
Differences between acceptors and rejectors in Switzerland emerged in terms of the perceived reliability of pediatricians [34]. Rejectors blamed mistrust on negative experiences with healthcare professionals [23,25,32]. Many GRTs reported experiencing regular discrimination and exclusion within the healthcare system, which generated hostility and discouraged use of health services [24]. Some hesitant Somali mothers in Sweden felt judged by healthcare professionals, and claimed they were denied more vaccine information. In one British study, mothers had less trust and a worse relationship with healthcare professionals who sent out vaccination reminders and questioned parents’ decisions not to vaccinate [23]. One Italian study showed vaccine-hesitant parents and rejectors were more likely to believe that healthcare professionals only gave information about the benefits of vaccination and neglected explaining the risks [29]. A British study showed mistrust in experts was blamed on inconsistent advice within the scientific community, with reference to research discrepancies such as Wakefield’s study [26].
On the other hand, most acceptors in British and Swedish studies mentioned specific experiences that fostered trust in healthcare professionals [23,28]. This Swedish study showed that acceptors followed immunization recommendations because they trusted experts [28]. Swedish parents with greater trust were more likely to vaccinate on time, dismiss MMR rumors, and ask more questions [25]. A questionnaire showed more acceptors and vaccine-hesitant parents in Italy considered their pediatrician to be competent, and to have spent enough time discussing MMR uptake, compared with rejectors [29].
3.4.2. Intentions
Parents expressed concern about commercial and societal motives behind vaccination promotion, with the suspicion that experts were motivated by generating profit [28,37]. Some mothers believed that healthcare professionals’ judgment could be clouded by financial incentives and performance targets [23]. Furthermore, one British study on rejectors highlighted a fear of government conspiracy, which was reinforced by the media attention given to the Prime Minister’s decision not to reveal the immunization status of his son [30].
3.4.3. Competence
Parents in one Swiss study frequently complained about the lack of high-quality, tailored advice to match their own skills and abilities [34]. Parents therefore felt they lacked competence in decision-making, so they based their decisions on social norms [34]. A British focus group highlighted that some mothers felt competent in decision-making through maternal instinct, which could override any advice [26]. However, some disagreed, claiming that vaccination decisions were beyond nurturing instincts [26].
3.5. Social Factors
3.5.1. Peer pressure
A reoccurring theme was perceived pressure and judgement from peers and family about parental knowledge, responsible parenting, and morals. All Somali mothers in a Swedish study claimed they were told about the link between MMR and autism by peers. Those who heard about vaccination without side effects chose to vaccinate, but those who heard experiences with adverse outcomes following vaccination chose to delay [25]. Some Swedish parents delayed vaccination due to perceived judgment by other parents who believed MMR is given too early [25]. Contrarily, some British mothers vaccinated due to fear of judgement from other acceptors [23]. Acceptors and rejectors expressed concerns about the knowledge and motivations of the opposing view [23].
3.5.2. Autonomy versus responsibility
The decision to vaccinate is a complex, time-consuming, and weighted decision, causing some to delay [28,38]. Acceptors acknowledged altruistically complying with official vaccination recommendations as social responsibility to protect the community [26,28]. Some mothers in a British study believed that complying with immunization recommendations should be a responsibility that comes with having children [26]. By conforming to national recommendations and accepting vaccination, hesitant mothers’ feelings of guilt and worry about potential consequences of MMR side effects were minimized as responsibility was shifted away from the mother [26]. Whereas vaccine-hesitant parents showed an individualistic outlook and justified this using the argument of autonomy [34]; choosing to refuse was perceived as an equally informed and responsible decision, however, guilt and worry about being responsible for their child’s risk of measles infection were still prevalent.
3.6. Practical Factors
3.6.1. Access
Practical barriers to vaccination associated with transient residency were highlighted in studies on GRT population in the UK [22,24]. GRT mothers claimed that regular travel resulted in a lack of knowledge of procedures, recommendations, and location of local clinics [22]. In some clinics, vaccination required a fixed address, so many GRT mothers were denied MMR [22,24]. Access was limited by lack of vehicle ownership and public transport in geographically isolated areas [22]. Geographic and social isolation of GRT communities excluded mothers from health promotion interventions. These factors magnified the lack of vaccination knowledge and increased reliance on informal sources of information [24]. Furthermore, a survey in Germany showed greater distance between the child’s home and the physician’s office negatively affected vaccination uptake [39].
3.6.2. Conflicting priorities
In a study assessing an MMR catch-up campaign in the UK, the acceptance of the first dose of measles vaccination was predicted by receipt of invitation, which acted as a reminder for parents who forgot to immunize [40]. In GRT communities, there were issues of fitting in immunization with competing needs and priorities [24]. Frequent child illness in these communities also caused delay or rejection of vaccination due to the contraindication of concurrent disease and MMR [24].
3.7. Knowledge Factors
3.7.1. Availability of information
Common sources of information existed across studies, although levels of trust differentiated between acceptors and rejectors. The main sources of knowledge were media coverage, internet, health professionals, and lay information. Rejectors were more likely to obtain information from lay sources and mass media, including newspapers, magazines, television, and internet, and claim to be influenced by them [30,31]. Family pediatricians were the most frequently consulted source of information for acceptors and vaccine-hesitant parents, but not for rejectors [29]. The availability of literature (such as posters, flyers, and brochures) at the physician’s office had no impact on vaccine attitudes. However, the use of patient management software to monitor vaccination uptake was associated with higher rates of immunization [39]. In GRT communities, mothers who had experienced MMR decision-making became the source of knowledge for other mothers [26]; this was especially prominent where there was little engagement with health services [24].
3.7.2. Reliability of information
Hesitant parents often felt frustrated with the lack of unbiased and accurate information [23,28], and rejectors more commonly reported receiving discordant opinions [29]. A large percentage of participants in two British studies who received catch-up invitations or leaflets felt they were not clear and informative enough [26,33].
3.7.3. Beliefs and worldviews
Parents of children in anthroposophical schools were significantly more influenced by alternative medicine, homeopathy, and natural remedies [27,39]. Somali mother acceptors felt confident in their decision as they believed that any consequence of vaccination was the will of God [25].
3.8. Demographics
Although the main focus of this review was attitudes and beliefs determining MMR uptake in parents, most studies attempted to record at least some influential demographic factors, such as age, education, ethnic group, number of children, and age of children. However, only eight studies discussed the implications of these, and few findings overlapped. One study in the UK found that younger and less deprived children, and children of an ethnic minority group were more likely to be vaccinated [40]. This was supported by another study in France that showed vaccine hesitancy to be lowest in parents of children aged 0–9 years [41]. Furthermore, mothers of unvaccinated children in an Italian study frequently had more children, and often took the decision to refuse MMR on the second-born rather than the first [31]. None of the studies assessed the intersection of income and education on MMR uptake, but rather examined these factors independently. One study conducted in the UK found that affluent parents were more hesitant and easily influenced by alternative health beliefs [32]. A study in France showed parents with a higher education were more hesitant [41], and a German study showed higher MMR coverage in populations with lower education [39]. Thus, vaccine hesitancy can be observed at both high and low educational levels. Age was also assessed; younger parents in Germany tended to support MMR vaccination more than older parents [39]. The association between the parents and physician’s age showed that younger parents are less likely to immunize if their physicians are older, and older parents are more likely to have immunized their children if the doctor was of similar age [39].
4. DISCUSSION
Using MacDonald’s 3C model of vaccine hesitancy [14], the six key themes identified in this systematic review can be categorized into three main categories: confidence, complacency, and convenience. Convenience is a particularly important category as not only does convenience determine enabling factors for vaccination but it also establishes barriers to vaccination regardless of parental desire to vaccinate. Complacency is most important when considering tailoring immunization strategies most effectively. However, the most important and most common theme that arose was fear about confidence of measles vaccination.
4.1. Confidence
MMR acceptors trusted vaccine safety, effectiveness, and experts. Accepting parents were more likely to be content with information given by experts. The main sources of knowledge were media coverage, internet, health professionals, and lay information. Family pediatricians were the most frequently consulted source of information for acceptors. Some parents were influenced by positive past experiences with vaccination. Hesitant parents felt pushed to vaccinate in fear of judgement by peers who have immunized.
In contrast, the main concerns of rejectors and vaccine-hesitant parents were fear of adverse effects resulting from MMR vaccination, which was mentioned in relation to autism in nine of the studies (45%). Parents expressed concerns about combination vaccines, fear of needles and pain, and young age for MMR administration. There was a significant lack of trust in experts and their possible motivations, which was shaped by experiences, perceived judgment, and unclear or inconsistent information. In communities with anthroposophical worldviews, there was greater trust in alternative medicine or natural remedies. Peer judgement, responsibility, and guilt both encouraged and discouraged uptake. Sources of information for hesitant parents and rejectors were more likely to stem from media and lay perspectives.
4.2. Complacency
Hesitant parents perceived measles to be low risk and non-severe. Rejectors, especially in anthroposophical communities, preferred natural development of the immune system or prioritized natural measures to avoid measles. Some hesitant parents delayed due to the importance of such a high-impact decision. On the other hand, acceptors believed measles was severe and felt responsibility to protect their child and the community.
4.3. Convenience
Cost was not an issue as MMR are covered by national immunization programs. Cost was an issue for GRT mothers who preferred spacing vaccination individually. Some parents simply forgot to immunize. Conversely, some accepting mothers followed recommendations to avoid the responsibility of making the decision themselves.
Although this review intentionally focused on parental attitudes toward measles vaccines in light of the current measles crisis in Europe, many findings were paralleled in systematic reviews on attitudes regarding general childhood vaccines in Europe [42,43]. The main difference was the unique fear of MMR and autism. The association between MMR and autism were discussed in almost half (n = 9) of the reviewed studies, despite Wakefield’s study having been published over 20 years ago and since been disproven. Although Wakefield’s study was conducted in the UK, its effects have extended to other European countries. This underlines the long-lasting, high impact of media coverage in portraying risk, information, and misinformation. Rejectors were more likely to be influenced by lay information and the media, making this an ideal medium to effectively reach the target population and correct misinterpretations and ambiguous information.
We found some discrepant findings regarding parental education. German and French studies found higher education to be associated with hesitancy [39,41], which may be because parents with higher education are more likely to question effectiveness and adverse effects of MMR. An Italian study supported this, showing that parents with lower education were less likely to search for information [38]. Therefore, poor knowledge about MMR may cause parents to feel less competent in decision-making. In contrast, Tabacchi’s meta-analysis of demographic predictors for parental MMR uptake showed that parents with lower education and lower incomes were much less likely to vaccinate their children with MMR [44]. Parents with high incomes were more than twice as likely to vaccinate and those with high education levels were 1.5 times as likely [44].
4.4. Confidence in Healthcare Providers and Systems
Acceptors were more likely to trust their healthcare provider and felt they had spent enough time discussing uptake compared with rejectors [29]. Healthcare professionals therefore have the responsibility to allocate sufficient time to allow parents to feel competent in decision-making. However, one study in Germany showed that too much time discussing MMR discouraged uptake, emphasizing the balance required to make this effective [39]. Furthermore, mothers, particularly from ethnic minority groups, felt discriminated and judged by experts based on their decision not to vaccinate, which worsened physician–patient relationships [23–25,32]. Healthcare environments should therefore be nondiscriminatory and fully inclusive of all communities and minorities. Physicians should aim to understand individual reasons for decisions, and tailor communication to target their unique experiences, beliefs, and attitudes, making information more relevant, trustworthy, and impactful [45]. The aim, therefore, is to move away from a ‘one-size-fits-all’ policy and provide an individualized approach to encourage evidence-informed decisions. For example, parents concerned about combined vaccination should first be properly informed about safety and risks, and subsequently offered separate immunization as necessary.
4.5. Barriers
A more proactive approach is needed to target hard-to-reach communities. The WHO identified surveillance to be more effective at highlighting susceptible populations by using decentralized health systems and subnational data, in comparison to centralized systems that use generalized national data and therefore often overlook problematic areas which are only discovered after an outbreak [46]. This is because factors leading to vaccine hesitancy are unevenly distributed within countries, leading to clusters of under-vaccinated populations at subnational levels. Countries with decentralized health systems could lead to different subnational strategies and vaccine promotion that result in varying vaccine uptake within the country. Therefore, public health surveillance must prioritize identifying clusters of rejectors and hesitant populations through vaccine registers and epidemiological research on demographic predictors for uptake. This paper highlighted certain vulnerable populations; large families, lower income, GRT, Orthodox, and anthroposophical populations. Subsequently, research is needed to diagnose barriers for vaccination in these groups.
The review showed that GRT mothers understood the value of immunization, however, were restricted by practical barriers, such as access, transient residency, and competing priorities [22]. To overcome this, community outreach programs should regularly offer health promotion and vaccination to these hard-to-reach populations [47]. Improving and maintaining high MMR coverage also involves adequate surveillance and monitoring; this helps to identify under-vaccinated populations, send reminders for vaccination, and monitor progress in immunization coverage.
5. STRENGTHS AND LIMITATIONS
This review has contributed to the existing literature on the European measles resurgence by providing a unique perspective on parental attitudes toward measles in Europe. This allows to develop better tools and strategies on how to most effectively shape and implement policies to improve vaccine uptake. This study focused on measles vaccine, thus limiting the possibility to compare our results with other reviews that focus on childhood vaccinations in general. Therefore, certain populations of rejectors of all vaccines were not included in this review, such as Orthodox populations. Furthermore, articles included in the review were limited to seven European countries, and consequently cannot be generalized across Europe or extrapolated to other contexts. These seven countries did not represent the highest or lowest incidence of measles, thereby potentially overlooking key determinants for uptake. The absence of qualitative studies on vaccine hesitancy in other European studies suggests that those countries may not be proactive in addressing measles vaccine uptake. Moreover, the search was limited to English publications, which may have affected the sensitivity of searches in other European languages.
6. CONCLUSION
Currently, all countries in Europe are experiencing a resurgence of measles, which has a detrimental effect on public health. Plans-Rubio’s study found low measles vaccination coverage to be the main driver [10]. Therefore, EVAP is currently not on schedule to achieve its goal of measles elimination by 2020, and as a result, the population is unnecessarily suffering from a preventable disease [4]. This review found that the most prominent barrier to vaccination was the lack of confidence in vaccine safety, in particular, the assumed causal relationship between MMR and autism. Skepticism was also evident in vaccine-hesitant parents who chose to delay based on age or stage of development. Furthermore, parents lacked confidence due to perceived judgement by peers. Fear of financial motivations and mistrust in experts were further reasons for hesitancy. Negative experiences with healthcare professionals, particularly in GRT populations experiencing discrimination, further caused mistrust. Anthroposophical populations had greater trust in natural remedies and lifestyles in preventing illness. Orthodox populations opposed vaccination based on religious convictions. Complacency of vaccine uptake was evident through perceived lack of severity and likelihood of measles infection; therefore, some parents only vaccinated during outbreaks. Many believed the risks of vaccination were greater than the severity of measles. Some parents, especially from anthroposophical communities, believed measles was a necessary part of natural child development. Lack of convenience was most frequently reported in GRT mothers with practical barriers, such as social and geographical isolation, resulting in lack of access to local clinics, transient residency, or inadequate knowledge about national recommendations. Furthermore, this population often experienced bouts of illness and competing priorities. Some parents simply forgot to immunize.
The complex, multidimensional decision-making process behind vaccination underpins the need for multilevel policy intervention. Previous successful campaigns have shown that for effective intervention, the disease must be well-known and feared, and vaccination should be accessible to all. First, healthcare professionals should use an individualistic and nonjudgmental approach to understand contextual reasons for vaccine decisions, to tailor effective communication, and to maintain trust. Furthermore, improved surveillance and monitoring is needed to identify under-vaccinated populations, and tailor vaccination programs to those subpopulations. National governments are responsible for redefining priorities to improve measles vaccination coverage. This multi-interventional, evidence-based approach is vital to improve parental confidence, competence, and convenience of measles vaccination uptake. Maintaining measles vaccination coverage consistently above 95% across and within countries in Europe will allow regional measles elimination to become a reality.
CONFLICTS OF INTEREST
The authors declare they have no conflicts of interest.
AUTHORS’ CONTRIBUTION
ABW-S and KQ did study conceptualization and wrote (review and editing) the manuscript. ABW-S did the data curation, formal analysis, and writing (original draft). ABW-S did the ethical approval request, and planned the investigation and methodology, with supervision and project administration by KQ. Resources and software sourced by ABW-S.
APPENDIX 1. PRISMA CHECKLIST
| Section/topic | # | Checklist item | Reported on page # |
|---|---|---|---|
| TITLE | |||
| Title | 1 | Identify the report as a systematic review, meta-analysis, or both. | 1 |
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number. | 2 |
| INTRODUCTION | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. | 3 |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS). | 4 |
| METHODS | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g., Web address), and, if available, provide registration information including registration number. | 5 |
| Eligibility criteria | 6 | Specify study characteristics (e.g., PICOS, length of follow-up) and report characteristics (e.g., years considered, language, publication status) used as criteria for eligibility, giving rationale. | 4/5 Figure 2 |
| Information sources | 7 | Describe all information sources (e.g., databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched. | 4/5 |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated. | Figure 1 |
| Study selection | 9 | State the process for selecting studies (i.e., screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis). | 4/5 Figure 1/2 |
| Data collection process | 10 | Describe method of data extraction from reports (e.g., piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators. | 5 |
| Data items | 11 | List and define all variables for which data were sought (e.g., PICOS, funding sources) and any assumptions and simplifications made. | 5 |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis. | 5 |
| Summary measures | 13 | State the principal summary measures (e.g., risk ratio, difference in means). | 5 |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (e.g., I2) for each meta-analysis. | 5 |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g., publication bias, selective reporting within studies). | 5 |
| Additional analyses | 16 | Describe methods of additional analyses (e.g., sensitivity or subgroup analyses, meta-regression), if done, indicating which were pre-specified. | n/a |
| RESULTS | |||
| Study selection | 17 | Give numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram. | Figure 2 |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g., study size, PICOS, follow-up period) and provide the citations. | Table 2 |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see Item 12). | Table 2 |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group (b) effect estimates and confidence intervals, ideally with a forest plot. | Table 2 |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency. | n/a |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see Item 15). | Table 2 |
| Additional analysis | 23 | Give results of additional analyses, if done (e.g., sensitivity or subgroup analyses, meta-regression [see Item 16]). | n/a |
| DISCUSSION | |||
| Summary of evidence | 24 | Summarize the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g., healthcare providers, users, and policy makers). | 6–10 Table 3/4 |
| Limitations | 25 | Discuss limitations at study and outcome level (e.g., risk of bias), and at review-level (e.g., incomplete retrieval of identified research, reporting bias). | 13/14 |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research. | 13–15 |
| FUNDING | |||
| Funding | 27 | Describe sources of funding for the systematic review and other support (e.g., supply of data); role of funders for the systematic review. | 15 |
REFERENCES
Cite this article
TY - JOUR AU - Annika B. Wilder-Smith AU - Kaveri Qureshi PY - 2019 DA - 2019/12/05 TI - Resurgence of Measles in Europe: A Systematic Review on Parental Attitudes and Beliefs of Measles Vaccine JO - Journal of Epidemiology and Global Health SP - 46 EP - 58 VL - 10 IS - 1 SN - 2210-6014 UR - https://doi.org/10.2991/jegh.k.191117.001 DO - 10.2991/jegh.k.191117.001 ID - Wilder-Smith2019 ER -
