HIV status, knowledge of mother-to-child transmission of HIV and antenatal care use among Ethiopian women
- DOI
- 10.1016/j.jegh.2014.01.001How to use a DOI?
- Keywords
- Human immunodeficiency virus; Knowledge; Prevention of mother-to-child transmission; Antenatal care; Ethiopia
- Abstract
Objective: To determine whether HIV status and knowledge of mother-to-child-transmission (MTCT) of HIV are associated with antenatal care (ANC) use.
Methods: Data were obtained from the 2011 Ethiopia Demographic and Health Survey among women aged 15–49 years who agreed to HIV testing and who reported giving birth in the preceding five years. The two exposures of interest were HIV status and knowledge of MTCT. Unadjusted and adjusted prevalence ratios for ANC use were estimated by fitting modified Poisson regression models.
Results: Among the 7392 women in the sample, ANC use was lowest among HIV-negative, low MTCT knowledge women (31.6% [95% confidence interval: 28.1–35.1]), and highest among HIV-positive, high knowledge women (81.9% [69.8–94.0%]). ANC use was significantly higher among HIV-positive, high knowledge (adjusted prevalence ratio [APR] = 1.60 [1.32–1.94]) and HIV-negative, high knowledge women (1.37 [1.24–1.51]) compared with HIV-negative, low knowledge women. There was no statistically significant difference in ANC use by HIV status among low knowledge women (1.26 [0.71–2.25]).
Conclusions: HIV-positive women generally had better MTCT knowledge. Among HIV-negative women, the prevalence of ANC use was greater among women with higher knowledge. Increasing MTCT knowledge may facilitate ANC use and in turn may eliminate MTCT.
- Copyright
- © 2014 Ministry of Health, Saudi Arabia. Published by Elsevier Ltd.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Introduction
The number of adults and children living with the human immunodeficiency virus (HIV) in sub-Saharan Africa has decreased from 2.2 million in 2001 to 1.8 million in 2009 [1]. However, women remain substantially affected by the epidemic in this region. In sub-Saharan Africa, young women aged 15–25 years are 8 times more likely than men to be HIV-positive [1]. With women of reproductive ages highly affected by HIV, identifying opportunities to prevent mother-to-child transmission (MTCT) of HIV is of utmost importance. Antenatal and postnatal services, where antiretroviral therapies (ART) can be provided to HIV-positive mothers to prevent transmission, represent an opportune setting to curb MTCT and achieve the World Health Organization (WHO) goal to eliminate MTCT by 2015 [1,2].
Ethiopia is among the sub-Saharan countries most affected by the HIV epidemic, with a prevalence of 1.5% among adults, and is among the 22 countries with the highest number of pregnant women living with HIV [2,3]. In recent years, the country has seen a 25% decline in new HIV infections in the general population based on ANC sentinel surveillance data, and there has been a decrease in HIV prevalence among women aged 15–24 years receiving antenatal care (ANC) [3–5]. Data from the 2011 Ethiopian Demographic and Health Survey (EDHS) also found that national general knowledge of the prevention of MTCT remains low [6]. At present, it remains unclear whether the observed decrease in HIV prevalence is due to a decline in HIV infection among pregnant women co-occurring with the decline in the general population, or instead that HIV-positive women have become less likely than HIV negative women to access ANC services.
HIV-positive status as well as low knowledge about MTCT may contribute to lower ANC use. Lower use of ANC services, particularly by HIV-positive women, hinders goals to eliminate MTCT. Therefore, the objective of this study was to determine whether HIV status and knowledge of MTCT are associated with ANC use among a national sample of Ethiopian women of reproductive age, 15–49 years.
2. Materials and methods
2.1. Source population
The data used for this analysis were obtained from the 2011 EDHS [7], a nationally representative cross-sectional survey conducted by the Central Statistical Agency (CSA), Ethiopia, and Macro International Inc., Calverton, Maryland, USA, as part of the MEASURE DHS project. HIV testing through the use of blood samples was conducted by the Ethiopia Health and Nutrition Research Institute. The survey sample was collected from December 2010 to June 2011 using a stratified, two-stage sample design from the Ethiopia 2007 Population and Health Census frame [6]. Each region was stratified into urban and rural areas and the two-stage sample selection was conducted independently within each sampling stratum. The first stage selected census enumeration units (EU), with the probability based on the EU size, and the second stage selected a fixed number of 30 households for each EU.
Three surveys were administered at sampled households: the Household Questionnaire, the Woman’s Questionnaire and the Man’s Questionnaire. The Household Questionnaire was used to gather household characteristics, to determine eligible men and women for the individual questionnaires, and to record the respondents that consented to give blood samples for HIV testing. All women aged 15–49 years were eligible for the Woman’s Questionnaire if they were usual residents of the household or were present the day of the survey and had slept in the selected household the night prior to the survey. HIV testing was done separately by EDHS biomarker technicians for those aged 15–49 years who voluntarily consented to the testing.
2.2. Study sample
The study sample consisted of women aged 15–49 years who at the time of the current EDHS agreed to HIV testing and reported a live birth in the five years since the last EDHS in 2005. Antenatal care data were available for women that reported having a live birth within the preceding 5 years of the current survey. Women were excluded from the analysis if blood results were not obtained or determined from the HIV test, and if women did not know if they had received antenatal care or if they refused to answer the question.
Among the 16,515 women interviewed for the 2011 EDHS, 15,517 (94.0%) had HIV test data available. Of these 15,517 women, 10,344 (66.7%) previously had a live birth; 7419 (71.7%) of the 10,344 women had a live birth within the last 5 years. Among these 7419 women, HIV status was missing for 4 women (0.1%), and 23 women (0.3%) did not have antenatal care data available. As a result, a total of 7392 women (7392/16,515 = 44.8%) met the study inclusion criteria.
2.3. Outcome variable
The outcome of interest was whether mothers received antenatal care for their last live birth within the preceding 5 years. Antenatal care was defined as “yes” if women responded with 1 or more to: “How many times did you receive antenatal care during this pregnancy?” Women who responded with 0 were defined as “no” and women who responded with “don’t know” were not included in the analysis.
2.4. Exposure variables
HIV status and knowledge of MTCT were the two primary exposure variables of interest. The survey contained one general question regarding AIDS (Q1:“Have you ever heard of an illness called AIDS?”) and four questions related to transmission of HIV: Q2: “Can the virus that causes AIDS be transmitted from a mother to her baby during pregnancy?”; Q3: “Can the virus that causes AIDS be transmitted from a mother to her baby during delivery?”; Q4: “Can the virus that causes AIDS be transmitted from a mother to her baby by breastfeeding?” and Q5: “Are there any special drugs that a doctor or a nurse can give to a woman infected with the AIDS virus to reduce the risk of transmission to the baby?”. All five questions were used to assess the level of knowledge. Questions included “yes”, “no”, and “don’t know” as potential responses. Responses to questions that were “don’t know” were included in the analysis as “No”. Out of 7392 women, there were 0, 1160, 1163, 910, and 1790 “don’t know” responses for Q1–Q5 respectively, and 6 missing responses for Q5.
A mother’s knowledge of MTCT was defined as “high” if she responded “yes” to 4 or more of the knowledge questions. Women who responded with “yes” to less than 4 questions were defined as “low” knowledge. The prior delimitation for the “high” knowledge category was chosen given that four corresponded to the median number of “yes” responses among HIV-negative and HIV-positive women.
A combined variable for HIV status and knowledge of MTCT was created for analysis as follows: HIV-positive, low knowledge; HIV-positive, high knowledge; HIV-negative, low knowledge and HIV-negative, high knowledge. Additional variables examined as potential confounders were current age (15–24 vs. 25–34 vs. ⩾35 years), place of residence (urban vs. rural), total number of live births in the last 5 years (1 vs. ⩾2), education (no education vs. ⩾primary education) and current marital status (not married vs. currently married).
2.5. Statistical analyses
A comparison of the distribution of categorical characteristics by HIV status and MTCT knowledge was conducted using χ2 tests. Unadjusted and adjusted modified Poisson regression models were used to estimate prevalence ratios (PR) for the association between HIV status-knowledge of MTCT and ANC use [8]. HIV-negative, low knowledge women were the reference group in primary analyses. Secondary analyses using the entire study sample were performed to better examine the association between HIV status and ANC use by the level of knowledge and the association between knowledge and ANC use by HIV status. HIV-positive, low knowledge and HIV-negative, high knowledge women were the reference groups in the secondary analyses.
All statistical tests were based on the weighted data. The following variables were considered to be potential confounders in the adjusted model based on previous findings of their association with HIV status, knowledge of MTCT and ANC use: age, place of residence, total number of live births in the last 5 years, education, and marital status [9–12]. All relevant variables were included as indicators in the unadjusted and adjusted models. The two-stage sampling structure was taken into account in the statistical analyses. A significance level of α = 0.05 was used and analyses were conducted with SAS version 9.3 (SAS Institute, Cary, North Carolina, USA).
3. Results
3.1. HIV status and knowledge
In this study sample of 7392 Ethiopian women, the prevalence of HIV was 1.4% (95% Confidence Interval: 1.0–1.8%) and the overall prevalence of high MTCT knowledge was 59.9% (57.3–62.5%). HIV status and MTCT knowledge were distributed as follows: 39.8% (37.2–42.3%) were HIV-negative with low knowledge, 58.9% (56.3–61.4%) were HIV-negative with high knowledge, 0.3% (0.1–0.5%) were HIV-positive with low knowledge and 1.0% (0.7–1.4%) were HIV-positive with high knowledge.
Table 1 shows the characteristics of women aged 15–49 years by HIV status and knowledge of MTCT. All examined characteristics were found to significantly differ by the HIV status/knowledge group. HIV-positive women were more likely to be aged 25–34 years compared with HIV-negative women. The HIV-positive, high knowledge group had a higher proportion of women living in an urban area and with a primary education or greater compared with HIV-positive women, low knowledge and HIV-negative women regardless of level of MTCT knowledge. HIV-negative women, regardless of their MTCT knowledge, had a higher proportion of 2 or more live births within the preceding 5 years compared with HIV-positive women. The majority of women in the study sample were married. Figs. 1 and 2 illustrate the distribution of MTCT knowledge by HIV status. Women that were HIV-positive generally had a higher proportion of “yes” responses to MTCT knowledge questions compared with HIV-negative women. A statistically significant higher proportion of the HIV-positive women compared with the HIV-negative women answered “yes” that HIV could be transmitted through pregnancy (78.4% [67.5–89.4%] vs. 62.6% [60.1–65.0%]) and that medications could be taken to avoid MTCT during pregnancy (67.5% [51.9–83.0%] vs. 36.2% [33.6–38.9%]). Furthermore, slightly more than half (59.0% [43.1–74.9%]) of the HIV-positive women answered “yes” to all five of the HIV-related questions, compared with 25.3% (23.2–27.4%) of the HIV-negative women (Fig. 2). Similarly, only 1.9% (0.0–5.5%) of the HIV-positive women answered “no” to all five of the HIV-related questions, compared with 4.2% (3.1–5.3%) of the HIV-negative women.
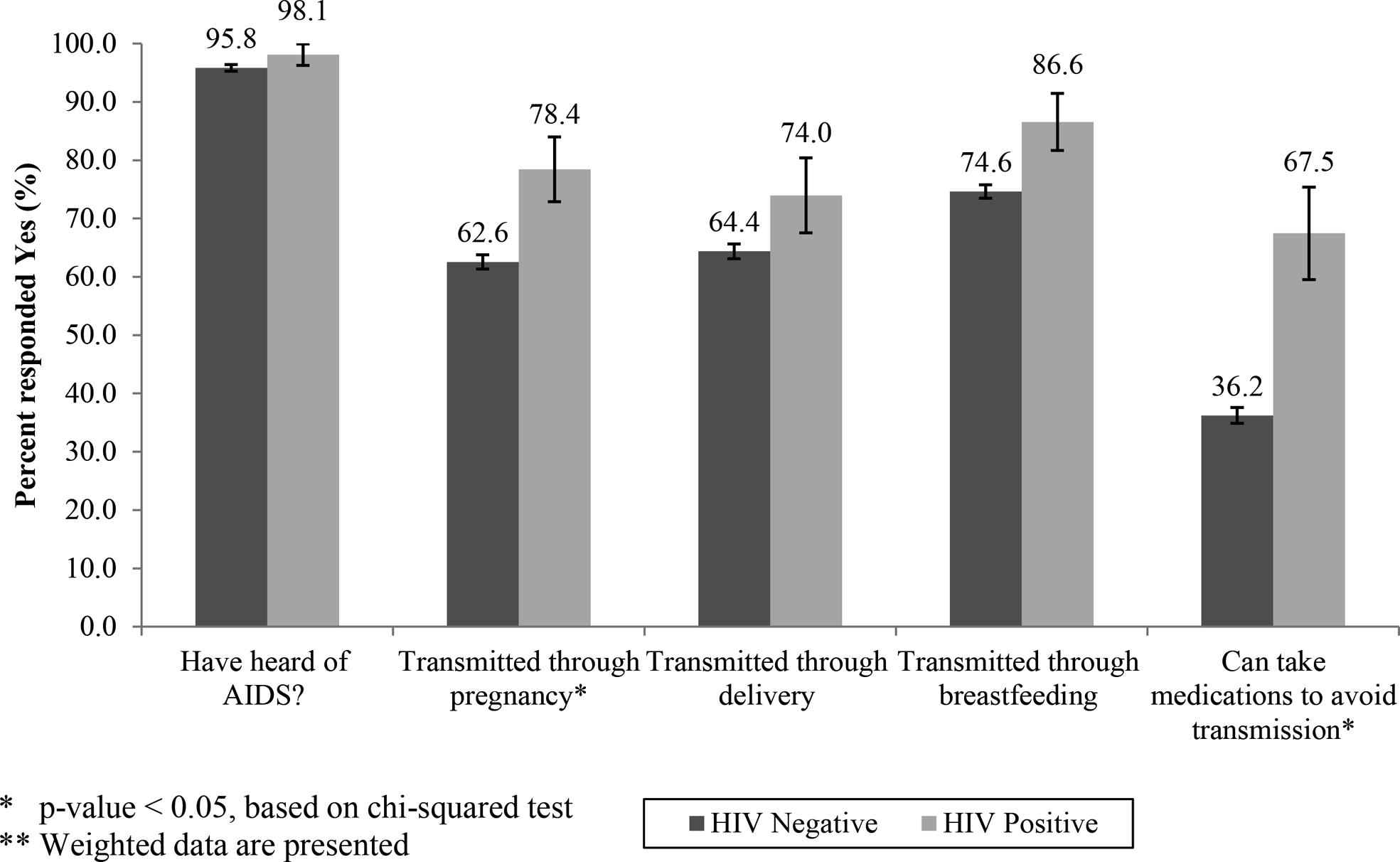
Knowledge of different methods of mother-to-child transmission of HIV by HIV status among 7392 women aged 15–49 years who had a live birth in the last 5 years, 2011 Ethiopian Demographic and Health Survey.**
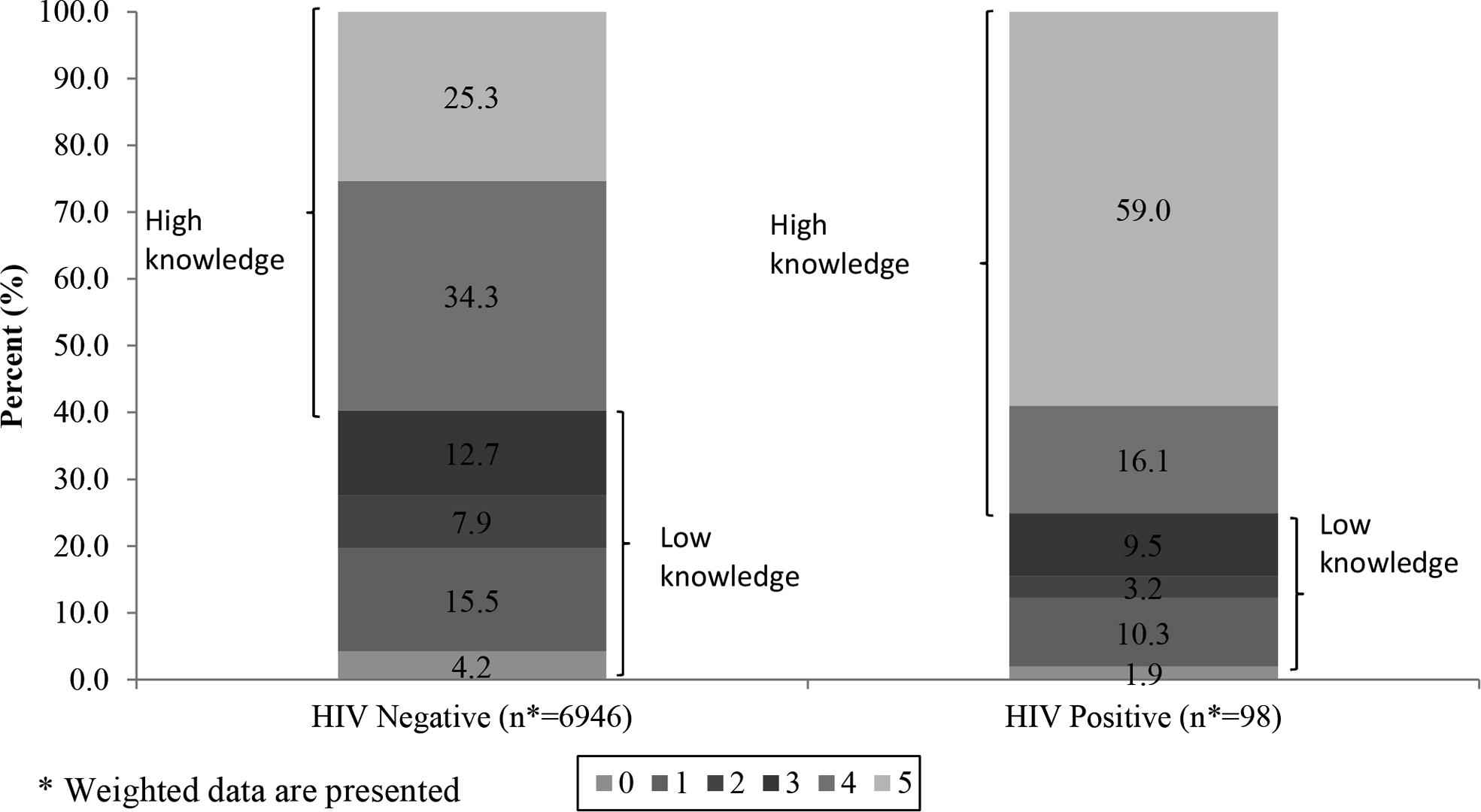
Number of “Yes” responses for the 5 HIV/AIDS related questions surveyed by HIV status among 7392 women aged 15–49 years who had a live birth in the last 5 years, 2011 Ethiopian Demographic and Health Survey.
| N Total | Weighted N total | HIV positive knowledge | HIV negative knowledge | p-valuea | |||
|---|---|---|---|---|---|---|---|
| High weighted N (%) | Low weighted N (%) | High weighted N (%) | Low weighted N (%) | ||||
| Age in years | 0.04 | ||||||
| 15–24 | 1930 | 1816 | 5 (7.4) | 3 (13.6) | 1065 (25.7) | 742 (26.5) | |
| 25–34 | 3586 | 3421 | 48 (65.2) | 19 (75.7) | 1991 (48.0) | 1363 (48.7) | |
| 35–49 | 1876 | 1808 | 20 (27.3) | 3 (10.7) | 1089 (26.3) | 695 (24.8) | |
| Residence | <0.01 | ||||||
| Urban | 1349 | 1031 | 52 (70.4) | 4 (16.6) | 754 (18.2) | 220 (7.9) | |
| Rural | 6043 | 6014 | 22 (29.6) | 20 (83.4) | 3392 (81.8) | 2580 (92.1) | |
| Total live births in the last 5 years | <0.01 | ||||||
| 1 | 4254 | 4005 | 59 (79.5) | 19 (76.1) | 2457 (59.3) | 1471 (52.5) | |
| 2 or more | 3138 | 3039 | 15 (20.5) | 6 (23.9) | 1689 (40.7) | 1329 (47.5) | |
| Highest educational level | <0.01 | ||||||
| No education | 4949 | 4696 | 23 (30.6) | 16 (65.9) | 2490 (60.1) | 2167 (77.4) | |
| Primary or greater | 2443 | 2349 | 51 (69.4) | 8 (34.1) | 1656 (39.9) | 634 (22.6) | |
| Current marital status | <0.01 | ||||||
| Not married | 685 | 645 | 22 (30.2) | 4 (15.0) | 386 (9.3) | 233 (8.3) | |
| Currently married | 6707 | 6400 | 51 (69.8) | 21 (85.0) | 3760 (90.7) | 2567 (91.7) | |
Chi-squared tests are based on weighted data.
Characteristics of 7392 women aged 15–49 years who had a live birth in the last 5 years by HIV status and knowledge of MTCT, 2011 Ethiopian Demographic and Health Survey.
3.2. Bivariate analysis
The prevalence of ANC use at the last live birth within the preceding 5 years was 42.9% (40.1–45.7%). ANC use was lowest among HIV-negative, low MTCT knowledge women (31.6% [28.1–35.1%]), followed by HIV-negative, high MTCT knowledge women (49.8% [46.7–52.9%]) (Fig. 3). Similarly among HIV-positive women, ANC use was lowest among women with low MTCT knowledge (44.4% [16.2–72.6%]) yet still higher than HIV-negative women, and highest among women with high MTCT knowledge (81.9% [69.8–94.0%]).

Antenatal care use by HIV status and knowledge of mother-to-child transmission of HIV among 7392 women aged 15–49 years who had a live birth in the last 5 years, 2011 Ethiopian Demographic and Health Survey.*
In the unadjusted regression analysis, the prevalence of ANC use at the last live birth was 2.59 (2.15–3.13) times greater among HIV-positive, high knowledge women compared with HIV-negative, low knowledge women (Table 2). The prevalence of ANC use at the last live birth among HIV-positive, low knowledge and HIV-negative, high knowledge women was 1.41 (0.75–2.65) and 1.58 (1.42–1.76) times greater, respectively, compared with women who were HIV-negative, low knowledge (Table 2). In secondary analyses, the prevalence of ANC use was 1.85 (0.97–3.50) times greater for women with high knowledge compared with women with low knowledge among HIV-positive women. Among women with high knowledge, the prevalence of ANC use was 1.64 (1.41–1.92) times greater for HIV-positive women compared with HIV-negative women.
| Knowledge level | Unweighted proportion having used ANC (N/Total) | Unadjusted model | Adjusted modela | ||||
|---|---|---|---|---|---|---|---|
| PRb | 95% | CI | PRb | 95% | CI | ||
| HIV positive | |||||||
| High | 73/89 | 2.59 | 2.15 | 3.13 | 1.60 | 1.32 | 1.94 |
| Low | 15/27 | 1.41 | 0.75 | 2.65 | 1.26 | 0.71 | 2.25 |
| HIV negative | |||||||
| High | 2240/4254 | 1.58 | 1.42 | 1.76 | 1.37 | 1.24 | 1.51 |
| Low | 977/3022 | 1.0 (reference) | 1.0 (reference) | ||||
Adjusted for age, marital status, number of previous live births, education, and place of residence.
The unadjusted and adjusted prevalence ratios (PR) were based on the weighted data.
Unadjusted and adjusted estimates of the prevalence ratio for antenatal care use by HIV status and knowledge of MTCT among 7392 women aged 15–49 years who had a live birth in the last 5 years, 2011 Ethiopian Demographic and Health Survey.
3.3. Multivariable analysis
Table 2 shows the multivariable modified Poisson results after adjusting for age, marital status, number of previous live births, education level and place of residence. The adjusted prevalence of ANC use among HIV-positive, high knowledge women was 1.60 (1.32–1.94) times greater than among HIV-negative, low knowledge women. Furthermore, the adjusted prevalence of ANC use at the last birth among HIV-positive, low knowledge women and HIV-negative, high knowledge women was 1.26 (0.71–2.25) and 1.37 (1.24–1.51) times greater, respectively, compared with women who were HIV-negative, low knowledge. In secondary analyses, the adjusted prevalence of ANC use was 1.27 (0.72–2.25) times greater for women with high-knowledge compared with women with low knowledge of MTCT among HIV-positive women. Among women with high knowledge, the adjusted prevalence of ANC use was 1.17 (1.00–1.38) times greater for HIV-positive women compared with HIV-negative women.
4. Discussion
In this study of Ethiopian women, HIV-positive women generally had better knowledge of MTCT compared with HIV-negative women. Specifically, a higher proportion of HIV-positive women compared with HIV-negative women answered “yes” that HIV can be transmitted through pregnancy and that medication can be taken to avoid transmission. Less than half of the HIV-negative women answered “yes” that MTCT could be avoided with medication during pregnancy. Knowledge of MTCT was more evenly distributed among HIV-negative women compared with HIV-positive women where more than half of the HIV-positive women answered “yes” to all five HIV-related questions.
The adjusted results indicated that among HIV-negative women, knowledge of MTCT was significantly positively associated with antenatal care use. Although among HIV-positive women the prevalence of ANC use was greater among women with higher knowledge, this greater prevalence was not statistically significant. Similarly, although ANC use was higher among HIV-positive women regardless of knowledge, this higher ANC use was not found to be statistically significant.
Previously the EDHS showed that MTCT knowledge in the general population was 42% in 2011 [6]. A cross-sectional study performed in 2011 among pregnant women attending a health institution in Gondar, Ethiopia, found that 88.5% knew of MTCT and 58.4% of women knew MTCT could be prevented by taking medication during pregnancy [10]. The findings in the present study that ANC use was greater among women with higher knowledge of MTCT are consistent with the prior cross-sectional survey that reported higher knowledge of MTCT among women in a healthcare setting compared with national EDHS estimates. Conversely, a study conducted in 2009 among pregnant women attending prevention of MTCT services in Southern Ethiopia found only 15.0% of women knew that delivery in a health facility, HIV treatment and avoiding breastfeeding were methods to prevent MTCT to the infant [12].
Knowledge of MTCT may not only play an important role in ANC use, but may also contribute to whether a woman participates in prevention of MTCT services once she is at a health facility [13,14]. Two studies conducted in 2008 in Ethiopian health institutions found that pregnant women with low knowledge of MTCT were less likely to use voluntary counseling and testing services [13,14], which is important in determining the woman’s HIV status and for providing her with HIV treatment. The potential link between MTCT knowledge, ANC use, and utilizing prevention of MTCT services once at the antenatal clinic is important given recent results from an analysis of a 5-year national level prevention of MTCT data from 2006 to 2010 in Ethiopia. This recent 5-year analysis found that 47% of HIV-positive pregnant women and 62% of exposed infants were still without ART [4]. These results demonstrate that providing treatment once HIV-positive mothers are at an ANC site still remains a challenge [3,4]. Increasing knowledge of MTCT among pregnant women may address this remaining public health challenge.
ANC use was higher among HIV-positive women than among HIV-negative women. However, the difference in ANC use was not statistically significant. These results may hint that the observed decrease in HIV prevalence among women aged 15–24 years receiving antenatal care is due to the recent 25% decline in new HIV infections [3,4] rather than HIV-positive women being less likely than HIV-negative women to access ANC services.
A number of limitations of the present study should be noted. First, the data are cross-sectional, thereby not allowing for the assessment of temporality that is necessary for proving causation. Secondly, type and quality of ANC use was not evaluated in this study, such as whether care was received from a skilled provider. In addition, given that prior research has shown that prevention of MTCT services is not available at all ANC service sites, these findings serve as a preliminary study, and future investigations will need to evaluate the types of ANC services used within HIV status and MTCT knowledge subgroups.
Thirdly, there was a small sample size of HIV-positive women that likely reduced the power to find statistically significant differences in ANC use by HIV status as well as by knowledge among HIV-positive women. Fourthly, the self-reported nature of the knowledge and ANC use questions may lead to social desirability bias. For example, given that almost 92% of the women in this study knew their HIV status at the time of their questioning, mothers who were HIV-positive may have been more inclined to respond “yes” to more of the transmission method questions regardless of their true knowledge level for fear of negative judgment from the interviewer. Both HIV-positive and HIV-negative mothers may have also been more likely to answer “yes” if respondents assumed that yes was the right, more desirable response.
However, there are several strengths to this analysis. This study was among the first to use a nationally representative sample to examine MTCT knowledge by HIV status. Assessing knowledge by HIV status is informative for public health efforts aimed at measuring and increasing awareness of prevention of MTCT among HIV-positive women. Furthermore, there are a limited number of studies that have examined HIV status or knowledge of MTCT as a predictor of ANC use using national level data such as the present study. Lastly, modified Poisson regression models were used to directly estimate prevalence ratios for ANC use rather than odds ratios where the odds ratio can overestimate the prevalence ratio in the setting of non-rare outcomes such as in this study [8].
5. Conclusions
In summary, these results provide preliminary evidence that higher MTCT knowledge may increase the likelihood of ANC use, certainly among HIV-negative women and likely among HIV-positive women as well. Future work should examine the association between HIV-positive status, knowledge of MTCT, and ANC use based on prospective rather than cross-sectional data. The association between knowledge and participation in prevention of HIV transmission services at antenatal care sites should also be prospectively evaluated in future studies.
Competing interests
There were no competing interests.
Funding disclosure
The Graduate School, the Department of Epidemiology, and the Richard B. Salomon Faculty Research Award at Brown University.
Conflict of interest
None declared.
Acknowledgements
The authors would like to thank Measure DHS for providing the data used in this study. We would especially like to thank Bridgette Wellington for providing assistance with the data.
References
Cite this article
TY - JOUR AU - Ida Sahlu AU - Chanelle J. Howe AU - Melissa A. Clark AU - Brandon D.L. Marshall PY - 2014 DA - 2014/02/13 TI - HIV status, knowledge of mother-to-child transmission of HIV and antenatal care use among Ethiopian women JO - Journal of Epidemiology and Global Health SP - 177 EP - 184 VL - 4 IS - 3 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2014.01.001 DO - 10.1016/j.jegh.2014.01.001 ID - Sahlu2014 ER -
