Putting surveillance data into context: The role of health care utilization surveys in understanding population burden of pneumonia in developing countries
Present address: New York City Department of Health and Mental Hygiene, New York, NY, USA.
- DOI
- 10.1016/j.jegh.2012.03.001How to use a DOI?
- Keywords
- Pneumonia; Comparative study; Patient acceptance of health care; Population surveillance; Health care
- Abstract
Background: Surveillance is essential to estimating the global burden of pneumonia, yet differences in surveillance methodology and health care-seeking behaviors limit inter-country comparisons.
Methods: Results were compared from community surveys measuring health care-seeking for pneumonia defined as: (1) cough and difficulty breathing for ⩾2 days; or, (2) provider-diagnosed pneumonia. Surveys were conducted in six sites in Guatemala, Kenya and Thailand; these sites also conduct, active, hospital- and population-based disease surveillance for pneumonia.
Results: Frequency of self-reported pneumonia during the preceding year ranged from 1.1% (Thailand) to 6.3% (Guatemala) and was highest in children aged <5 years and in urban sites. The proportion of persons with pneumonia who sought hospital-based medical services ranged from 12% (Guatemala, Kenya) to 80% (Thailand) and was highest in children <5 years of age. Hospitals and private provider offices were the most common places where persons with pneumonia sought health care. The most commonly cited reasons for not seeking health care were: (a) mild illness; (b) already recovering; and (3) cost of treatment.
Conclusions: Health care-seeking patterns varied widely across countries. Using results from standardized health care utilization surveys to adjust facility-based surveillance estimates of pneumonia allows for more accurate and comparable estimates.
- Copyright
- © 2012 Published by Elsevier Ltd. on behalf of Ministry of Health, Saudi Arabia.
- Open Access
- This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/)
1. Introduction
Disease surveillance is essential for characterizing disease burden and defining public health priorities, monitoring and evaluating disease prevention programs and identifying outbreaks. However, comparison of disease burden estimates obtained from surveillance systems in place in different countries may be limited by differences in the surveillance methodologies within these countries. Surveillance for infectious diseases is typically based in hospitals and other health care facilities. Hospital-based surveillance is an efficient form of surveillance as it captures the more severe manifestations of the illness of interest and usually includes a standardized collection of objective data such as physical exam findings and laboratory diagnostic testing, enabling better adherence to a standardized case definition. In contrast, community-based surveillance – although less efficient and often more costly than hospital-based surveillance – enables earlier detection of the disease of interest and captures illnesses in persons who do not seek care in a hospital. Also, in many rural settings in developing countries, hospitals and other health care facilities may not be accessible to most persons living in a community due to the distance to the facility or the cost of care at such a facility.
Because of suspected differences in where and when communities seek medical care for various illnesses, disease burden estimates from hospital- or other facility-based surveillance in different countries or regions may not be comparable to one another, even if similar case definitions and surveillance methods are used. Therefore, proper interpretation of facility-based surveillance data – particularly between two or more countries – requires a thorough understanding of both the surveillance system and the population’s use of health care for the disease under study [1].
In most countries a wide range of health care options exist and include public and private hospitals, ambulatory care centers, pharmacies, drug sellers (people who sell medications in stores not designated as pharmacies) and traditional healers. Also, within a single community, health care-seeking patterns may vary by illness. Because of differences in health care-seeking behaviors, the proportion of the true burden of disease measured by health care facility-based surveillance may differ both between countries and within a single country. Community-wide health care utilization surveys characterize the health care-seeking behavior of ill persons by describing where ill persons sought health care for their illnesses, and soliciting reasons for not seeking health care.
The International Emerging Infections Program (IEIP) of the United States Centers for Disease Control and Prevention is a network of international sites that work with partners in the host countries to build local capacity to detect and respond to emerging infectious disease threats. A principal activity of each IEIP site is the establishment of surveillance for pneumonia and other influenza-like illnesses—leading killers of children worldwide [2]. Objectives of pneumonia surveillance in the IEIP sites are to estimate pneumonia incidence, characterize the leading etiologies of pneumonia, and track disease trends over time. In addition to initiating surveillance for severe respiratory infections and other select illnesses, the IEIP sites also conducted health care utilization surveys in the larger community surrounding the surveillance hospitals. These surveys were used to inform planning and implementation of facility-based surveillance systems and as a tool to adjust crude calculations of incidence from surveillance data toward more accurate estimates of disease burden within communities under surveillance.
In this paper, the health care utilization patterns for persons with pneumonia in three countries – Guatemala, Kenya and Thailand – where IEIP conducts population-based surveillance are compared. These data can be used to help guide the establishment of effective surveillance systems, improve national disease burden estimates, and ultimately contribute to more accurate global disease burden estimates.
2. Materials and methods
2.1. Surveillance sites and survey methods
From 2003 through 2009, six community-wide health care utilization surveys were conducted at two sites in each of the three countries: Guatemala, Kenya and Thailand (Fig. 1). Findings from several of these surveys have been published [3–8]. In Guatemala one survey was conducted in the Department of Santa Rosa (pop. 308,522; 14% <5 years old), located in the southeastern part of the country, while the second survey was conducted in Quetzaltenango (pop. 705,301; 14% <5 years old), located in western Guatemala. The two Thailand sites were based in the agrarian, rural provinces of Sa Kaeo (pop. 509,337; 7% <5 years old), in eastern Thailand, and Nakhon Phanom (pop. 715,549; 8% <5 years old), located in the Northeast. The Kenyan sites included Kibera, an urban slum in Nairobi (Gatwikira and Soweto villages, pop. 29,015; 15% <5 years old), and Rarieda (formerly known as Bondo), a rural district in western Kenya (pop. 24,000; 15% <5 years old). The surveys were conducted in 2003 (Sa Kaeo), 2005 (Nakhon Phanom, Rarieda and Kibera), 2006 (Santa Rosa) and 2009 (Quetzaltenango).
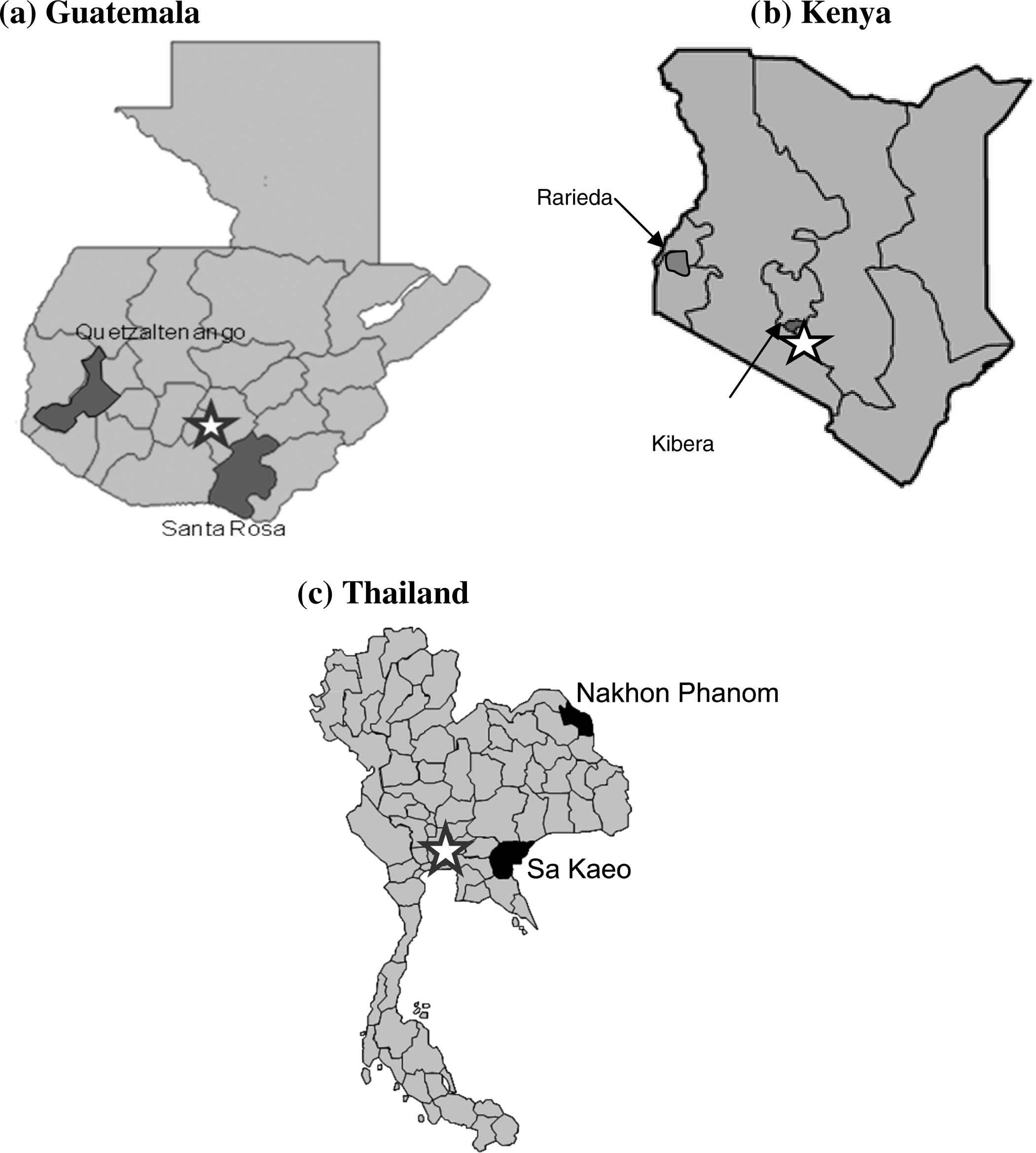
Location of study sites in (a) Guatemala; (b) Kenya; and (c) Thailand. (The star represents the county’s capital).
Persons of all ages were included in the community surveys except those in Kenya, which were restricted to members of households with at least one child aged <5 years. The case definition of pneumonia used in the surveys was adapted from the World Health Organization (WHO) verbal autopsy report for severe pneumonia in children, using questions that were moderately sensitive and specific for pneumonia [9]. In Guatemala and Thailand, pneumonia was defined as self-reported cough and difficulty breathing for ⩾2 days or diagnosis of pneumonia by a health care provider during the past 12 months. In Kenya, pneumonia was defined as cough and difficulty breathing for >2 days (Rarieda) or >5 days (Kibera) or diagnosis of pneumonia by a health care provider in the past 12 months, excluding the past two weeks. The rationale stated for excluding respiratory illness during the two weeks prior to interview was the hypothesis that respiratory illness episodes in the past two weeks were more likely to be reported and magnified in severity because they were still fresh in the minds of the respondents [10].
The method for selecting households in which to conduct the surveys was based on the cluster survey approach used to estimate community immunization coverage and adapted for each survey site [11]. In Kenya, a one-stage cluster sampling approach was used. Villages were selected using probability proportional to size sampling, and all households with a child aged <5 years and located within each village were selected. A two-stage cluster sampling was used in the surveys conducted in Thailand and Santa Rosa. In the first stage, villages were selected using probability proportional to size sampling. In the second stage, 20–40 households were randomly selected within each of the selected villages. A stratified simple random sample was used in urban Quetzaltenango; households were selected using geospatial sampling (households nearest to randomly generated coordinates in each sampled area) methodology.
In all surveys a similar interviewer-administered questionnaire was used to collect household demographic information and information for all individuals living in the household. The head of household or primary caretaker served as a proxy for all household members. Households were excluded if the head of household or primary caregiver refused to participate or if the head of household or primary caregiver was unavailable for interview. In addition to asking if the household members had self-reported or physician-diagnosed pneumonia in the previous 12 months, participants with a history of pneumonia were asked if they sought medical care for themselves or their children for an episode of pneumonia. Other places where health care was sought or reasons for not seeking health care were also ascertained.
Each survey protocol was approved by the Institutional Review Boards of the United States Centers for Disease Control and Prevention and by a local academic or Ministry of Health Institutional Review Board.
2.2. Analysis
For each study population, household characteristics and household member demographics were characterized. The frequency of pneumonia was calculated for each study population overall and by age group and sex. The percentage of persons with pneumonia who sought hospital-based care (inpatient and outpatient) was determined. Statistical analyses were performed using SAS/SUDAAN (SAS Institute Inc., Cary, NC; SUDAAN Research Triangle Inc., Raleigh, NC) in Thailand and Kenya, SPSS/SUDAAN (SPSS Inc., Somers, NY) in Santa Rosa, Guatemala, and STATA in Quetzaltenango, Guatemala (StatCorp LP, College Station, TX); 95% confidence intervals (CI) were calculated using the Taylor series linearization method (Quetzaltenango, Santa Rosa, Rarieda and Nakhon Phanom), the inverse Fisher F probability function (Kibera) and Fleiss quadratic 95% CI for a cluster sample (Sa Kaeo).
To demonstrate how health care utilization survey data can be used to adjust facility-based rates of pneumonia obtained from routine, existing surveillance, mean estimates of health care-seeking in children aged <5 years were used to adjust previously reported incidence rates of hospitalized pneumonia for similarly aged children in Kenya and Thailand where facility-based rates were available. In Rarieda, Kenya, the previously reported pneumonia incidence was based on physician diagnosis listed in the admission log books [12]. In Thailand, previously reported pneumonia incidence was based on a standard surveillance definition (at least one sign or symptom of acute infection, at least one sign or symptom of lower respiratory tract infection and chest radiographic findings consistent with pneumonia) [4]. Rates were then adjusted using the percentage of children with pneumonia who visited a hospital for care. The subsequently adjusted rate assumes that all children meeting survey criteria for pneumonia were sick enough either to have been referred to a hospital or to have been admitted to a hospital.
3. Results
3.1. Health care utilization surveys
Descriptions of households are shown in Table 1. The median household size was larger in Guatemala and Kenya than in Thailand. The estimated percentage of household participants with reported pneumonia occurring during the previous 12 months within each surveillance population (all ages included) ranged from 1.1% in Sa Kaeo, Thailand to 6.3% in Santa Rosa, Guatemala (Table 2). At each site, pneumonia frequency was higher among children aged <5 years when compared with persons aged ⩾5 years.
| Guatemala | Kenya | Thailand | ||||
|---|---|---|---|---|---|---|
| Santa Rosa | Quetzaltenango | Rarieda | Kibera | Nakhon Phanom | Sa Kaeo | |
| Household characteristics | ||||||
| Households that completed a survey, n (% of total households chosen) | 1131 (94) | 1851 (88) | 981 (97) | 1818 (87) | 2000 (100) | 1598 (99.9) |
| Median household size (range) | 4.8 (1–20) | 5 (1–18) | 5 (2–17) | 5 (2–18) | 4 (1–15) | 3 (1–12) |
| Caregiver education is ⩽primary schoola (%) (95% CI) | 78 (76–81) | 68 (53–83) | 88 (86–90) | 81 (78–84) | 56 (54–58) | 86 (84–88) |
| Households with at least one child age <5 years (%) (95% CI) | 40 (37–43) | 37 (33–40) | 100 (–)b | 100 (–)b | 28 (26–30) | 22 (20–25) |
| Individual characteristics | ||||||
| Total persons assessed in screening interview, n | 5449 | 9668 | 6223 | 9110 | 7724 | 5658 |
| Age group in years (%) surveyedc | ||||||
| <5 | 11 | 9.3 | 27b | 31b | 8.4 | 7.2 |
| 5–18 | 36 | 38 | 36 | 28 | 25 | 28 |
| 19–64 | 47 | 48 | 36 | 42 | 58 | 57 |
| ⩾65 | 5.6 | 5.3 | 1.2 | <0.1 | 8.4 | 7.9 |
| Male (%) surveyed | 48 | 48 | 48 | 49 | 47 | 50 |
Kenya: <primary school.
Household criteria for inclusion in HUS was presence of one or more children aged <5 years.
Percents may add up to >100 because of rounding.
Characteristics of households and individuals completing health care utilization survey in Guatemala, Kenya and Thailand.
| Pneumonia status | Guatemala | Kenyab | Thailand | |||
|---|---|---|---|---|---|---|
| Santa Rosa (%) (95% CI) | Quetzaltenango (%) (95% CI) | Rarieda (%) (95% CI) | Kibera (%) (95% CI) | Nakhon Phanom (%) (95% CI) | Sa Kaeo (%) (95% CI) | |
| Reported pneumonia | ||||||
| All ages | 6.3 (5.6–6.9) | 1.4 (0.9–1.9) | 2.5 (2.1–2.9) | 5.7 (5.2–6.2) | 1.8 (1.5–2.1) | 1.1 (0.8–1.5) |
| <5 years | 11 (8.9–13) | 3.7 (2.4–5.0) | 2.7 (2.2–3.3) | 8.9 (7.9–10) | 9.9 (7.8–12.5) | 4.9 (2.8–8.4) |
| ⩾5 years | 5.6 (5.0–6.3) | 1.2 (0.7–1.6) | 2.1 (1.6–2.8) | 4.3 (3.8–4.8) | 1.0 (0.8–1.3) | 0.7 (0.5–1.1) |
| Male | 6.5 (5.6–7.5) | 1.3 (0.9–1.7) | 2.2 (1.7–2.8) | 5.9 (5.2–6.6)c | 1.9 (1.5–2.4) | 1.4 (0.9–2.1) |
| Female | 6.0 (5.1–6.9) | 1.5 (0.8–2.1) | 2.7 (2.2–3.4) | 5.6 (5.0–6.3)c | 1.7 (1.3–2.1) | 0.7 (0.4–1.2) |
| Persons with pneumonia who sought hospital carea | ||||||
| All ages | 8.4 (6.0–11) | 24 (13–34) | 41 (31–52) | 17 (14–21) | 58 (50–67) | 80 (67–89) |
| <5 years | 15 (4.7–24) | 39 (23–56) | 48 (34–62) | 19 (14–23) | 52 (40–65) | 85 (55–97) |
| ⩾5 years | 6.8 (4.4–9.3) | 19 (10–28) | 34 (22–48) | 15 (12–19) | 64 (52–74) | 77 (56–90) |
| Male | 8.5 (5.9–11) | 25 (12–38) | 45 (30–61) | 16 (12–20) | 62 (50–68) | 77 (56–90) |
| Female | 8.3 (5.9–11) | 23 (12–34) | 39 (27–53) | 18 (14–23) | 55 (44–61) | 85 (55–97) |
All sites except Kenya excluded persons who sought care outside the catchment area.
Kenya survey inclusion criteria included household with one or more children <5 years of age.
Estimated percentages.
Frequency of self-reported pneumonia in previous 12 months among persons surveyed by age group and sex (Guatemala, Kenya and Thailand).
The proportion of persons of all ages with pneumonia who sought hospital-based care varied widely between study sites, from 8% in Santa Rosa, Guatemala to 80% in Sa Kaeo, Thailand (Table 2). The proportion of all persons with pneumonia who sought hospital-based care varied up to 22% between two sites within one country. Except in Nakhon Phanom, Thailand, hospital-based care for children aged <5 years was sought more frequently than for people aged ⩾5 years.
Hospitals and private providers were the most common places persons with pneumonia sought health care (Table 3). Seeking treatment from pharmacists/drug sellers was more common in Kenya (38–42%) than at the other sites (1.5–16%), and seeking health care from health centers or dispensaries was more common in Rarieda, Kenya (⩾55%) than at the other sites (9–34%).
| Where care was soughta | Guatemala | Kenya | Thailand | |||
|---|---|---|---|---|---|---|
| Santa Rosa (%) (95% CI) | Quetzaltenango (%) (95% CI) | Rarieda (%) (95% CI)c | Kibera (%) (95% CI) | Nakhon Phanom (%) (95% CI) | Sa Kaeo (%) (95% CI) | |
| Hospital | 8.4 (6.0–11) | 59 (43–76) | 41 (31–52) | 17 (14–21) | 58 (50–67) | 80 (67–89) |
| Outpatient | – | – | 24 (16–34) | 13 (9.9–16) | 52 (43–61) | 68 (50–82) |
| Emergency | 4.1 (2.6–5.5) | – | – | – | 9.1 (5–15) | 3.8 (0.4–18) |
| Inpatient | – | – | 21 (14–31) | 4.0 (3.1–5.0) | – | 21 (10–38) |
| Private physician or clinic | 28 (26–29) | 47 (38–57) | 28 (20–39) | 20 (18–23) | 55 (46–63) | 55 (37–71) |
| Pharmacist or drug seller | 11 (9.1–13) | 13 (6.3–21) | 38 (20–38) | 42 (39–46) | 1.5 (0.4–5.9) | 9.4 (2.7–25) |
| Health volunteer | – | 0.9 (<0.1–2.7) | 3.0 (0.9–9.2) | 1.7 (0.3–3.1) | 0 | 1.9 (0.0–15) |
| Health center or clinic | 11 (9.8–12) | 18 (8.6–27) | 55 (46–64) | 30 (27–33) | 15 (10–23) | 34 (19–52) |
| Health post/dispensary | 11 (9.2–13) | – | –b | –b | – | – |
| Religious leader | – | – | – | 12 (9.6–14) | 0 | 0 |
| Traditional healer | 4.4 (3.6–5.2) | 2.7 (<0.1–6.9) | 7.0 (3.2–14) | – | 0 | 0 |
“–” Indicates that the health care site was not included as a possible response for where persons seek health care.
Categories are not mutually exclusive.
Combined with “Health center or clinic”.
Patterns of health care-seeking among persons reporting pneumonia in the past 12 months in Guatemala, Kenya and Thailand.
Few persons with pneumonia did not seek some level of health care for their illness. The percentage of persons who did not seek health care was greatest at both Guatemala sites (21% in Santa Rosa, 17% in Quetzaltenango vs. ⩽8% at any of the other sites). In Guatemala, the most commonly cited reasons for not seeking health care for pneumonia were not being sick enough (40%) and costs of treatment (16%).
3.2. Adjusting incidence of hospitalized pneumonia
Between 2001 and 2003, the annual rate of hospitalized pneumonia among children aged <5 years in Rarieda, Kenya was 698 per 100,000 population [12]. The survey data indicate that 48% of pneumonia episodes among children in this community would present to a hospital for care. Therefore, the adjusted incidence rate of pneumonia was 1,454 per 100,000 children aged <5 years.
Between 2002 and 2004, the rate of hospitalized pneumonia among children aged <5 years in Nakhon Phanom and Sa Kaeo, Thailand was 2,783 and 1,893, respectively. Our survey data indicate that 52% and 85%, respectively, of pneumonia episodes among children in these communities would present to a hospital for care. The adjusted incidence rates for pneumonia was therefore 5,321 (Nakhon Phanom) and 2,227 (Sa Kaeo) per 100,000 children aged <5 years. Estimates of the annual rate of hospitalized pneumonia among children aged <5 years in Guatemala are not available to calculate the adjusted incidence rate for the two sites in this country.
4. Discussion
Because pneumonia is the leading cause of death in children worldwide, this study aimed to characterize health care utilization in children aged <5 years [2]. At the majority of study sites, a higher percentage of children aged <5 years with pneumonia sought hospital care than did persons aged 5 years or older. Nakhon Phanom, Thailand was the only study site where hospital-based care for children aged <5 years with pneumonia was sought less frequently than for persons aged 5 years or older. Data from a study comparing health care-seeking behavior for pneumonia in Nakhon Phanom and Sa Kaeo, Thailand found that children <5 years of age in Nakhon Phanom were more likely to have had an episode of pneumonia reported than their Sa Kaeo counterparts. This suggests that differences in health care-seeking behaviors among children <5 years may be attributed to perceived severity of illness or differences in accessibility of hospital care. The lower percentage of people aged ⩾5 years with pneumonia who sought hospital-based care suggests that in most sites the incidence of adults with pneumonia as calculated from facility-based surveillance alone will also be underestimated.
In recent years there have been comprehensive efforts to estimate the global burden of disease due to a number of respiratory pathogens, yet these estimates are driven largely by incidence data derived from facility-based surveillance [13–15]. As the data suggest, in many parts of the world a substantial proportion of persons with pneumonia may never seek care at a hospital. Understanding these differences in health care-seeking behaviors and making data-driven adjustments to crude incidence calculations may result in more accurate global disease estimates.
This study found that a significantly higher proportion of persons in both Thailand sites and Quetzaltenango, Guatemala (range 58–80%) sought hospital care for pneumonia when compared with the other study sites (range 8–41%). Differences in socioeconomic status likely explain some of these differences and, in fact, Kenyans who did not seek care reported the cost of treatment as the number one reason for not seeking care [7]. The distance to a hospital, although infrequently reported in these surveys, also has been shown to play an important role in seeking medical services [16–18].
Some of these findings have already influenced the implementation of population-based surveillance. The health care utilization survey conducted in Santa Rosa indicated that private physicians were treating approximately 36% of severe respiratory illnesses. As a result, the Guatemalan Ministry of Public Health and IEIP expanded active surveillance to include private providers. The health care utilization survey conducted in Rarieda indicated that using clinic-based surveillance alone to define disease rates would sufficiently underestimate pneumonia frequency, supporting the decision to implement home-based surveillance [5]. In contrast, hospital-based surveillance in Thailand continued unchanged, based primarily on the finding that the majority of persons with self-reported pneumonia sought hospital care. This surveillance system was subsequently used to highlight the importance of influenza as a cause of hospitalized pneumonia in Thailand, which in turn helped guide the vaccine policy in this country [19].
This analysis of health care utilization surveys had several limitations. First, the specificity of the case definition for defining a pneumonia episode is unknown. Self-reported pneumonia is a difficult syndrome to standardize, and the surveys in these study may have captured milder acute respiratory illness syndromes that was not consistent with pneumonia, which might have led to an overestimate of the number of pneumonia cases missed by hospital-based surveillance. Conversely, recall of an illness in the previous 12 months may be difficult, especially if the illness was mild, therefore leading to underestimation of the number of persons with pneumonia who did not seek care at a hospital. Secondly, although the written definition of pneumonia was similar between sites, local interpretation may have been different, leading to across-site variability in what was being reported as pneumonia. Researchers in Kenya also used a different sampling scheme, limiting data collection to households with at least one child aged <5 years, which may have led to a bias in the sample of adults with respect to pneumonia prevalence and health care-seeking behaviors. Thirdly, various attention-grabbing outbreaks of respiratory disease, including Severe Acute Respiratory Syndrome (SARS), avian influenza A (H5N1) and 2009 pandemic influenza A (H1N1) occurred during some of the study periods [20–23]. While not necessarily increasing the frequency of pneumonia, these outbreaks may have increased awareness and thus reporting of respiratory disease; they also may have changed health care-seeking behaviors. Finally, surveys may have been influenced by whether respondents deemed a particular response to be the “correct” answer in the eyes of an interviewer working with the Ministry of Health or an international organization. Respondents may have been more likely to indicate that they would seek care at a clinic or hospital (even if they would not) or that they would not seek care from a traditional medicine provider (even if they would).
Global respiratory disease surveillance continues to inform public health decisions and guide prevention measures, particularly estimates of the magnitude of an infection in a community or country. Understanding health care-seeking behaviors is important to optimal interpretation of surveillance data at the local, national and global levels. The impact of particular socioeconomic and cultural factors within communities on health care utilization should be carefully considered, and may be best ascertained by health care utilization surveys.
5. Conclusions
Patterns of health care utilization for pneumonia varied significantly between countries and between sites within the same country. The diversity in health care-seeking patterns likely reflects a combination of factors, including local traditions, location of health care facilities, availability of local transportation, ratio of hospitals to population size, access to health insurance, and general wealth in a country [3,4,6,7]. Measuring the differences in health care utilization allows for a more accurate interpretation of surveillance results and thus enables a comparison of the magnitude of the burden of pneumonia across sites as estimated from surveillance data. Facility-based surveillance estimates in Thailand and Kenya were adjusted and resulted in a 1.2- to 2-fold higher estimated incidence for pneumonia in children aged <5 years.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
References
Cite this article
TY - JOUR AU - Meredith Deutscher AU - Chris Van Beneden AU - Deron Burton AU - Alvin Shultz AU - Oliver W. Morgan AU - Shadi Chamany AU - Hannah T. Jordan AU - Xingyou Zhang AU - Brendan Flannery AU - Daniel R. Feikin AU - Beatrice Olack AU - Kim A. Lindblade AU - Robert F. Breiman AU - Sonja J. Olsen PY - 2012 DA - 2012/05/22 TI - Putting surveillance data into context: The role of health care utilization surveys in understanding population burden of pneumonia in developing countries JO - Journal of Epidemiology and Global Health SP - 73 EP - 81 VL - 2 IS - 2 SN - 2210-6014 UR - https://doi.org/10.1016/j.jegh.2012.03.001 DO - 10.1016/j.jegh.2012.03.001 ID - Deutscher2012 ER -
