Bilateral lower extremity arterial thromboembolism mimicking conversion disorder
- DOI
- 10.1016/j.artres.2012.11.003How to use a DOI?
- Keywords
- Arterial thromboembolism; Conversion disorder; Arteriography
- Abstract
Thromboembolic causes of acute limb ischemia are not frequent; however, an immediate true therapy is needed to save the extremity. Here we presented a case with bilateral lower extremity arterial thromboembolism mimicking conversion disorder. Conversion disorder and acute arterial embolism can be confronted in different patterns. This case proved us that anamnesis can be misleading and manipulating to evaluate patients. Furthermore, our report may potentially highlight the inadequacies in the guidelines for diagnosis.
- Copyright
- © 2012 Association for Research into Arterial Structure and Physiology. Published by Elsevier B.V. All rights reserved.
- Open Access
- This is an open access article distributed under the CC BY-NC license.
Introduction
Thromboembolic causes of acute limb ischemia are not frequent; however, an immediate true therapy is needed to save the extremity. Although epidemiological studies are insufficient, the incidence of acute peripheral arterial occlusion (APAO) is 14/100,000.1 The cases are seldom bilateral (6%).2 This disease may cause life-threatening complications besides loss of extremity. Literature reports 10%–25% mortality rate and 20% amputation rate.3,4 Arterial emboli are the most common cause of acute peripheral arterial occlusions and mostly originate from the heart.5 It is known that ischemic complications are more often seen in the cases treated after 8 h of occlusion.4 We presented a case with anamnesis of conversion disorder and bilateral thromboembolism.
Case report
A 42-year old female presented to emergency department complained of approximate 10 h of ongoing sciatic nerve tracing, right buttock pain radiating to leg, and nausea. The patient was assaulted and hit in the lower limb by her husband. Despite she was agitated nearby relatives, she was calm while alone. Besides, it was observed that she usually appealed to the emergency department with this kind of right sciatic nerve pain and crying spells.
The physical examination revealed no pathological findings on initial evaluation. Peripheral arterial pulses were palpable in both lower extremities. Pallor, motor-sensory loss, swelling, deformity, redness, and tenderness were not observed. A normal sinus rhythm was available in electrocardiography, and blood tests were normal.
After about 1 h, the right leg was cold and no pulses were found. In the left lower extremity, none of coldness, pallor, and pain was observed, and peripheral arterial pulses were weak. Pelvic arteriography was performed, and bilateral acute arterial occlusion of the lower extremity was diagnosed.
In arteriogram, there were filling defects at the distal part of the right common iliac artery, and at the internal and external iliac arteries, whereas the appearance of the arteries were normal at the left side. The arteriogram also showed poor filling of the right superficial femoral and popliteal arteries (Fig. 1). However, there were filling defects at the tibioperoneal trunk, proximal part of the peroneal artery and anterior tibial artery (Fig. 2a and b). The posterior tibial artery was patent, and the poor filling of the peroneal artery was observed. However, there were no flow at the right crural arteries and the left anterior tibial artery except the proximal part of the left anterior tibial artery (Fig. 3a and b).
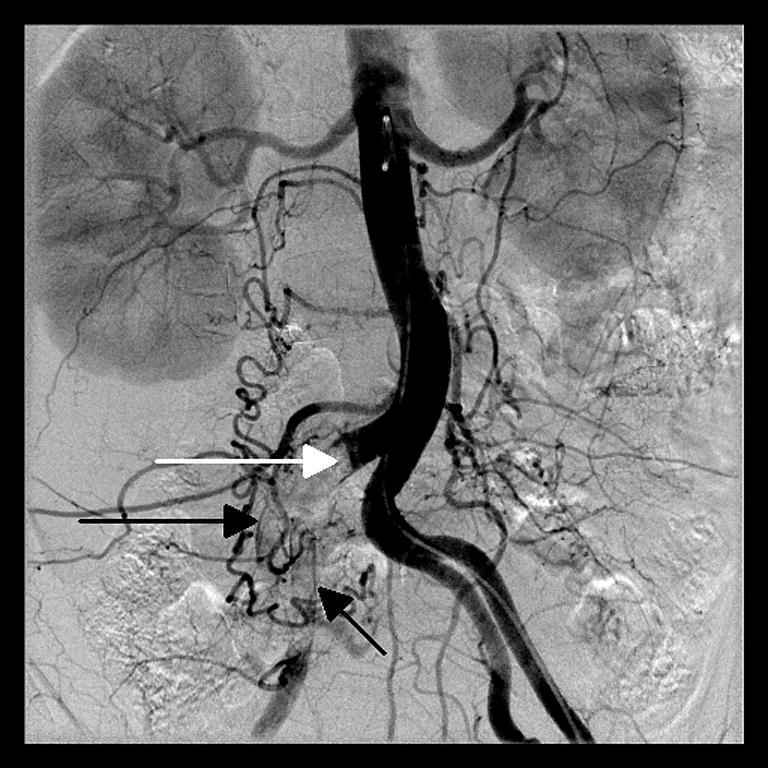
In arteriogram, there were filling defects at the distal part of the right common iliac artery (white arrow), and internal (short black arrow) and external (long black arrow) iliac arteries, whereas the appearance of the arteries were normal at the left side.

a and b. Arteriogram showed poor filling of the right superficial femoral artery (a) and popliteal artery (b) (arrows).
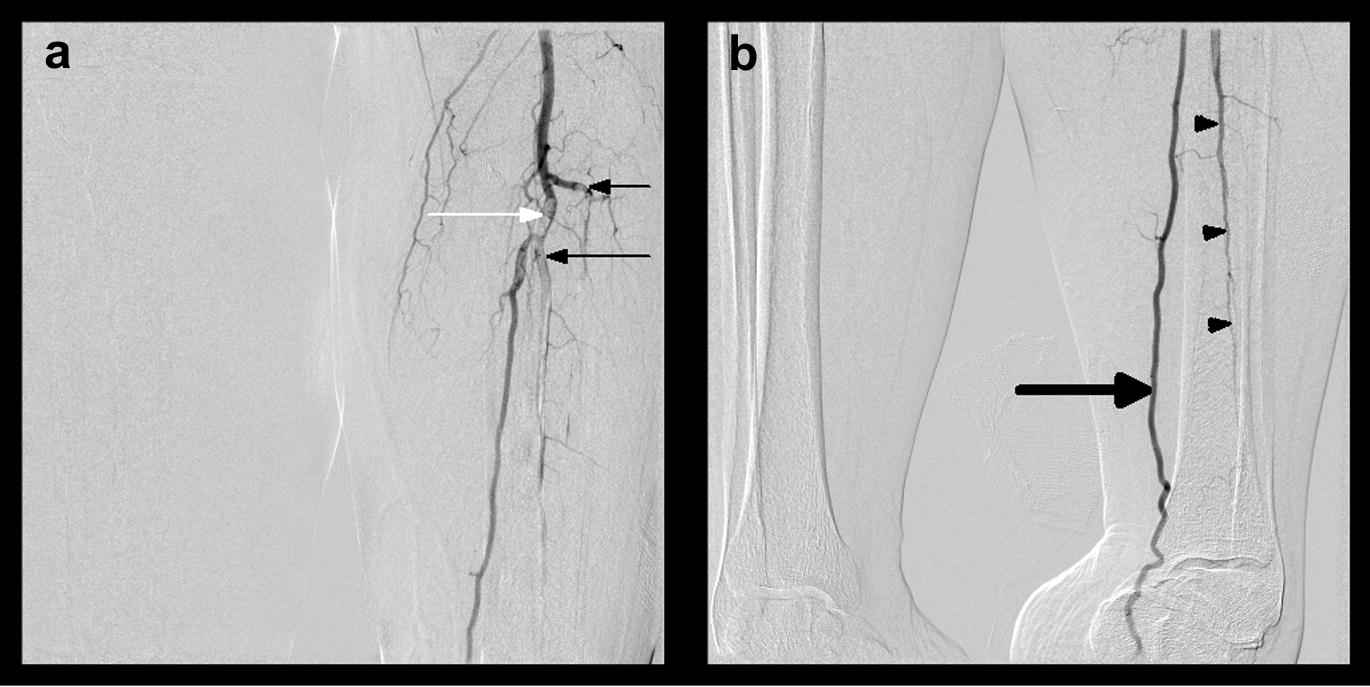
a and b. Arteriogram showed that there were filling defects at the tibioperoneal trunk (white arrow), at the proximal part of the peroneal artery (long black arrow), and at the anterior tibial artery (short black arrow). The posterior tibial artery was patent (thick arrow) and the poor filling of peroneal artery was shown (arrowheads). However, there was no flow at the right crural arteries and the left anterior tibial artery except the proximal part of the left side.
Later, the patient was operated on, and an embolectomy was performed on the right leg, while medical treatment was enough for the left side. The origin of embolus was not found, and the patient was discharged after 10 days of operation.
Discussion
Conversion disorder, usually following severe stress, manifests itself with various nonspecific symptoms such as paralysis, aphonia, dyskinesia, presyncope, pseudoseizures, and so on. Thus, conversion disorder mimicks many organic pathologies. It is reported that a significant number of patients with organic pathologies (2%–50%) are misdiagnosed with conversion disorder.6,7 Our case, diagnosed with APAO, had a story of emergency department presence with complaints of agitation, crying, being beaten, and a post-assault increase in the patient’s pre-existing sciatic pain. She became calm while alone despite the agitated nearby relatives. Therefore, conversion disorder was considered first.
“6P” findings (pallor, pulselessness, perishing cold, pain, paresthesia, and paralysis) have a significant role in APAO.3 Findings in the cases presented included sudden severe pain in the leg, numbness, coldness, paleness, and pulselessness.8,9 However, the main APAO symptoms and findings were not present in our case when the patient presented to the emergency department.
Peripheral nerves and skeletal muscles are the tissues most sensitive to ischemia. Irreversible changes take place as a result of 6 h exposure to anoxia at the room temperature.3 In the cases when the length of time from the beginning of the complaints is less than 12 h, the extremity conservation rate is 93% and the death rate is 19%. In the cases when the length of time is more than 12 h, the extremity conservation rate is diminished to 78% and the death rate escalates to 30%.10 In our case, it raised a suspicion of the anamnesis because the initial examination revealed no APAO findings although it was reported that 10 h had passed since the symptoms started. In the physical examination repeated after 1 h, the typical findings were observed to have developed.
Conclusion
Conversion disorder and acute arterial embolism can be confronted in different patterns. This APAO case proved us that anamnesis can be misleading and manipulating to evaluate patients. In differential diagnosis, physical examination should be done carefully without the influence of history. Furthermore, our report may potentially highlight the inadequacies in the guidelines for diagnosis.
References
Cite this article
TY - JOUR AU - Umut Yucel Cavus AU - Mahmut Nedim Aytekin AU - Sema Avci AU - Macit Aydin AU - Mehmet Sait Dogan PY - 2013 DA - 2013/01/02 TI - Bilateral lower extremity arterial thromboembolism mimicking conversion disorder JO - Artery Research SP - 103 EP - 105 VL - 7 IS - 2 SN - 1876-4401 UR - https://doi.org/10.1016/j.artres.2012.11.003 DO - 10.1016/j.artres.2012.11.003 ID - Cavus2013 ER -
